REVIEW PAPER
Wider perspective on Spinal Muscular Atrophy – pathogenesis, diagnosis, treatment
1
Student’s Scientific Society of Clinical Genetics, Medical University, Lublin, Poland
2
Department of Clinical Genetics, Medical University, Lublin, Poland
Corresponding author
Paulina Gil-Kulik
Department of Clinical Genetics, Medical University of Lublin, Radziwiłłowska 11 Street, 20-080, Lublin, Romania
Department of Clinical Genetics, Medical University of Lublin, Radziwiłłowska 11 Street, 20-080, Lublin, Romania
J Pre Clin Clin Res. 2024;18(4):358-364
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
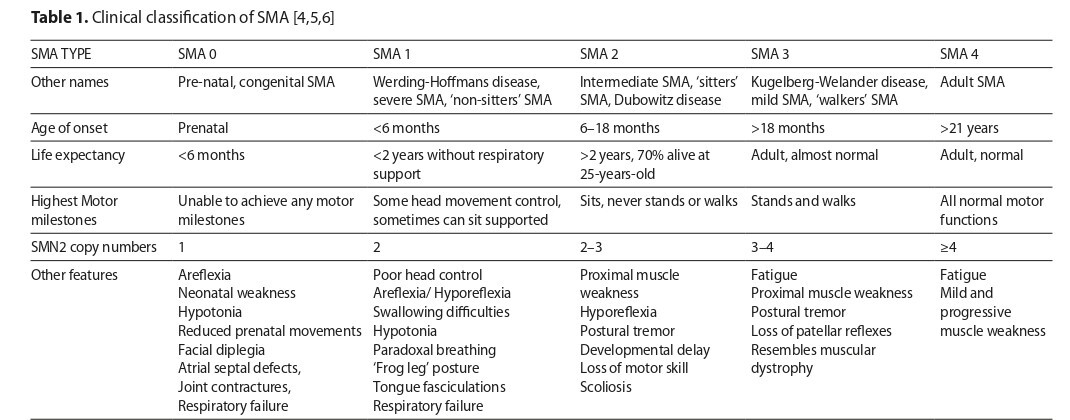
Spinal muscular atrophy (SMA) is an autosomal recessive inherited disease that leads to the atrophy or weakening of skeletal muscles and changes in the brainstem. It is the second most common cause of infant mortality worldwide, with a prevalence ranging from about 1 in 6,000 to 1 in 10,000 live births. The cause of the disease is the presence of mutations in the survival motor neuron 1 (SMN1) gene on chromosome 5q11.2 to 13.3. The aim of this review is to summarize and compile the current state of knowledge on SMA, including its pathogenesis, diagnosis and treatment.
Review methods:
The review is based on scientific publications found in the PubMed, Scopus, and Google Scholar databases, published between 2018–2024.
Brief description of the state of knowledge:
Genetic testing for SMA is the most accurate method, demonstrating a 100% positive predictive value. To determine disease severity, the number of SMN2 gene copies is analyzed, while carrier detection involves analyzing copies of the SMN1 gene. Clinical trials evaluated using the HFMSE scale demonstrated significant improvements in motor function with risdiplam, apitegromab, and nusinersen. Onasemnogene abeparvovec was assessed using the CHOP INTEND scale, also showed improvements in motor function
Summary:
Treating SMA presents a significant challenge for doctors, as selecting the appropriate therapy and timing its introduction are crucial. Currently, the FDA-approved drugs include nusinersen, onasemnogene abeparvovec, and risdiplam
Spinal muscular atrophy (SMA) is an autosomal recessive inherited disease that leads to the atrophy or weakening of skeletal muscles and changes in the brainstem. It is the second most common cause of infant mortality worldwide, with a prevalence ranging from about 1 in 6,000 to 1 in 10,000 live births. The cause of the disease is the presence of mutations in the survival motor neuron 1 (SMN1) gene on chromosome 5q11.2 to 13.3. The aim of this review is to summarize and compile the current state of knowledge on SMA, including its pathogenesis, diagnosis and treatment.
Review methods:
The review is based on scientific publications found in the PubMed, Scopus, and Google Scholar databases, published between 2018–2024.
Brief description of the state of knowledge:
Genetic testing for SMA is the most accurate method, demonstrating a 100% positive predictive value. To determine disease severity, the number of SMN2 gene copies is analyzed, while carrier detection involves analyzing copies of the SMN1 gene. Clinical trials evaluated using the HFMSE scale demonstrated significant improvements in motor function with risdiplam, apitegromab, and nusinersen. Onasemnogene abeparvovec was assessed using the CHOP INTEND scale, also showed improvements in motor function
Summary:
Treating SMA presents a significant challenge for doctors, as selecting the appropriate therapy and timing its introduction are crucial. Currently, the FDA-approved drugs include nusinersen, onasemnogene abeparvovec, and risdiplam
Daniłowska K, Picheta N, Piekarz J, Pobideł J, Gil-Kulik P. Wider Perspective on Spinal Muscular Atrophy – Pathogenesis, Diagnosis, Treatment. J Pre-Clin Clin Res. 2024; 18(4): 358–364. doi: 10.26444/jpccr/196213
REFERENCES (50)
1.
Butchbach MER. Genomic Variability in the Survival Motor Neuron Genes (SMN1 and SMN2): Implications for Spinal Muscular Atrophy Phenotype and Therapeutics Development. Int J Mol Sci. 2021;22(15):7896. doi:10.3390/ijms22157896
2.
Glascock J, Sampson J, Haidet-Phillips A, et al. Treatment Algorithm for Infants Diagnosed with Spinal Muscular Atrophy through Newborn Screening. J Neuromuscul Dis. 2018;5(2):145–158. doi:10.3233/JND- 180304.
3.
Wijngaarde CA, Stam M, Otto LAM, et al. Population-based analysis of survival in spinal muscular atrophy. Neurology. 2020;94(15):e1634-e1644. doi:10.1212/WNL.0000000000009248.
4.
Monani UR, Lorson CL, Parsons DW, et al. A single nucleotide difference that alters splicing patterns distinguishes the SMA gene SMN1 from the copy gene SMN2. Hum Mol Genet. 1999;8(7):1177–1183. doi:10.1093 hmg/8.7.1177.
5.
Mailman MD, Heinz JW, Papp AC, et al. Molecular analysis of spinal muscular atrophy and modification of the phenotype by SMN2. Genet Med. 2002;4(1):20–26. doi:10.1097/00125817-200201000-00004.
6.
Main M, Kairon H, Mercuri E, Muntoni F. The Hammersmith functional motor scale for children with spinal muscular atrophy: a scale to test ability and monitor progress in children with limited ambulation. Eur J Paediatr Neurol. 2003;7(4):155–159. doi:10.1016/s1090-3798(03)00060-6.
7.
Šimić G, Vukić V, Babić M, et al. Total tau in cerebrospinal fluid detects treatment responders among spinal muscular atrophy types 1–3 patients treated with nusinersen. CNS Neurosci Ther. 2024;30(3):e14051. doi:10.1111/cns.14051.
8.
Anagnostou E, Miller SP, Guiot MC, et al. Type I spinal muscular atrophy can mimic sensory-motor axonal neuropathy. J Child Neurol. 2005;20(2):147–150. doi:10.1177/08830738050200022101.
9.
Sugarman EA, Nagan N, Zhu H, et al. Pan-ethnic carrier screening and prenatal diagnosis for spinal muscular atrophy: clinical laboratory analysis of >72,400 specimens. Eur J Hum Genet. 2012;20(1):27–32. doi:10.1038/ejhg.2011.134.
10.
Wang Y, Wang Z. Systematical identification of splicing regulatory cis-elements and cognate trans-factors. Methods. 2014;65(3):350–358. doi:10.1016/j.ymeth.2013.08.019.
11.
Zerres K, Rudnik-Schöneborn S. Natural history in proximal spinal muscular atrophy. Clinical analysis of 445 patients and suggestions for a modification of existing classifications. Arch Neurol. 1995;52(5):518–523. doi:10.1001/archneur.1995.00540290108025.
12.
Carissimi C, Saieva L, Gabanella F, Pellizzoni L. Gemin8 is required for the architecture and function of the survival motor neuron complex. J Biol Chem. 2006;281(48):37009–37016. doi:10.1074/jbc.M607505200.
13.
Alioto TS. U12DB: a database of orthologous U12-type spliceosomal introns. Nucleic Acids Res. 2007;35(Database issue):D110–D115. doi:10.1093/nar/gkl796.
14.
Luo M, Liu L, Peter I, et al. An Ashkenazi Jewish SMN1 haplotype specific to duplication alleles improves pan-ethnic carrier screening for spinal muscular atrophy. Genet Med. 2014;16(2):149–156. doi:10.1038/gim.2013.84.
15.
Clermont O, Burlet P, Lefebvre S, Bürglen L, Munnich A, Melki J. SMN gene deletions in adult-onset spinal muscular atrophy. Lancet. 1995;346(8991–8992):1712–1713. doi:10.1016/s0140-6736(95)92881-2.
16.
Wijaya YOS, Nishio H, Niba ETE, et al. Detection of Spinal Muscular Atrophy Patients Using Dried Saliva Spots. Genes. 2021;12(10):1621. doi:10.3390/genes12101621.
17.
Aasdev A, R S S, Iyer VR, Moharir SC. Spinal muscular atrophy: Molecular mechanism of pathogenesis, diagnosis, therapeutics, and clinical trials in the Indian context. J Biosci. 2024;49:36.
18.
Weisburd B, Sharma R, Pata V, et al. Detecting missed diagnoses of spinal muscular atrophy in genome, exome, and panel sequencing datasets. Published online February 13, 2024. doi:10.1101/2024.02.11.24302646.
19.
Freigang M, Steinacker P, Wurster CD, et al. Glial fibrillary acidic protein in cerebrospinal fluid of patients with spinal muscular atrophy. Ann Clin Transl Neurol. 2022;9(9):1437–1448. doi:10.1002/acn3.51645.
20.
Rich KA, Fox A, Yalvac M, et al. Neurofilament Levels in CSF and Serum in an Adult SMA Cohort Treated with Nusinersen. J Neuromuscul Dis. 2022;9(1):111–119. doi:10.3233/JND-210735.
21.
Šimić G, Vukić V, Babić M, et al. Total tau in cerebrospinal fluid detects treatment responders among spinal muscular atrophy types 1–3 patients treated with nusinersen. CNS Neurosci Ther. 2024;30(3):e14052. doi:10.1111/cns.14051.
22.
Hviid CVB, Madsen AT, Winther-Larsen A. Biological variation of serum neurofilament light chain. Clin Chem Lab Med CCLM. 2022;60(4):569–575. doi:10.1515/cclm-2020-1276.
23.
Smeriglio P, Langard P, Querin G, Biferi MG. The Identification of Novel Biomarkers Is Required to Improve Adult SMA Patient Stratification, Diagnosis and Treatment. J Pers Med. 2020;10(3):75. doi:10.3390/jpm10030075.
24.
Brown N. Atoms. Arch Dis Child. 2023;108(7):i-i. doi:10.1136/archdischild-2023-325895.
25.
Day JW, Howell K, Place A, et al. Advances and limitations for the treatment of spinal muscular atrophy. BMC Pediatr. 2022;22(1):632. doi:10.1186/s12887-022-03671-x.
26.
Lejman J, Panuciak K, Nowicka E, Mastalerczyk A, Wojciechowska K, Lejman M. Gene Therapy in ALS and SMA: Advances, Challenges and Perspectives. Int J Mol Sci. 2023;24(2):1130. doi:10.3390/ijms24021130.
27.
Mirea A, Leanca MC, Onose G, et al. Physical Therapy and Nusinersen Impact on Spinal Muscular Atrophy Rehabilitative Outcome. Front Biosci-Landmark. 2022;27(6):179. doi:10.31083/j.fbl2706179.
28.
Li Q. Nusinersen as a Therapeutic Agent for Spinal Muscular Atrophy. Yonsei Med J. 2020;61(4):273. doi:10.3349/ymj.2020.61.4.273.
29.
Łusakowska A, Wójcik A, Frączek A, et al. Long-term nusinersen treatment across a wide spectrum of spinal muscular atrophy severity: a real-world experience. Orphanet J Rare Dis. 2023;18(1):230. doi:10.1186/s13023-023-02769-4.
30.
Neil EE, Bisaccia EK. Nusinersen: A Novel Antisense Oligonucleotide for the Treatment of Spinal Muscular Atrophy. J Pediatr Pharmacol Ther. 2019;24(3):194–203. doi:10.5863/1551-6776-24.3.194.
31.
Migliorati JM, Liu S, Liu A, et al. Absorption, Distribution, Metabolism, and Excretion of US Food and Drug Administration–Approved Antisense Oligonucleotide Drugs. Drug Metab Dispos. 2022;50(6):888–897. doi:10.1124/dmd.121.000417.
32.
Darras BT, Farrar MA, Mercuri E, et al. An Integrated Safety Analysis of Infants and Children with Symptomatic Spinal Muscular Atrophy (SMA) Treated with Nusinersen in Seven Clinical Trials. CNS Drugs. 2019;33(9):919–932. doi:10.1007/s40263-019-00656-w.
33.
Acsadi G, Crawford TO, Müller-Felber W, et al. Safety and efficacy of nusinersen in spinal muscular atrophy: The EMBRACE study. Muscle Nerve. 2021;63(5):668–677. doi:10.1002/mus.27187.
35.
Ogbonmide T, Rathore R, Rangrej SB, et al. Gene Therapy for Spinal Muscular Atrophy (SMA): A Review of Current Challenges and Safety Considerations for Onasemnogene Abeparvovec (Zolgensma). Cureus. Published online March 15, 2023. doi:10.7759/cureus.36197.
36.
Blair HA. Onasemnogene Abeparvovec: A Review in Spinal Muscular Atrophy. CNS Drugs. 2022;36(9):995–1005. doi:10.1007/s40263-022-00941-1.
37.
Weiß C, Ziegler A, Becker LL, et al. Gene replacement therapy with onasemnogene abeparvovec in children with spinal muscular atrophy aged 24 months or younger and bodyweight up to 15 kg: an observational cohort study. Lancet Child Adolesc Health. 2022;6(1):17–27. doi:10.1016/S2352-4642(21)00287-X.
38.
Chand D, Mohr F, McMillan H, et al. Hepatotoxicity following administration of onasemnogene abeparvovec (AVXS-101) for the treatment of spinal muscular atrophy. J Hepatol. 2021;74(3):560–566. doi:10.1016/j.jhep.2020.11.001.
39.
New drug: Onasemnogene abeparvovec for spinal muscular atrophy. Aust Prescr. 2022;45(4):140–141. doi:10.18773/austprescr.2022.044.
40.
Day JW, Finkel RS, Chiriboga CA, et al. Onasemnogene abeparvovec gene therapy for symptomatic infantile-onset spinal muscular atrophy in patients with two copies of SMN2 (STR1VE): an open-label, single-arm, multicentre, phase 3 trial. Lancet Neurol. 2021;20(4):284–293. doi:10.1016/S1474-4422(21)00001-6.
41.
Strauss KA, Farrar MA, Muntoni F, et al. Onasemnogene abeparvovec for presymptomatic infants with two copies of SMN2 at risk for spinal muscular atrophy type 1: the Phase III SPR1NT trial. Nat Med. 2022;28(7):1381–1389. doi:10.1038/s41591-022-01866-4.
42.
Chaytow H, Faller KME, Huang YT, Gillingwater TH. Spinal muscular atrophy: From approved therapies to future therapeutic targets for personalized medicine. Cell Rep Med. 2021;2(7):100346. doi:10.1016/j.xcrm.2021.100346.
43.
Dhillon S. Risdiplam: First Approval. Drugs. 2020;80(17):1853–1858. doi:10.1007/s40265-020–01410-z.
45.
Risdiplam. Am J Health Syst Pharm. 2021;78(1):4–6. doi:10.1093/ajhp/zxaa347.
47.
Paik J. Risdiplam: A Review in Spinal Muscular Atrophy. CNS Drugs. 2022;36(4):401–410. doi:10.1007/s40263-022-00910-8.
48.
Baranello G, Darras BT, Day JW, et al. Risdiplam in Type 1 Spinal Muscular Atrophy. N Engl J Med. 2021;384(10):915–923. doi:10.1056/NEJMoa2009965.
49.
Oskoui M, Day JW, Deconinck N, et al. Two-year efficacy and safety of risdiplam in patients with type 2 or non-ambulant type 3 spinal muscular atrophy (SMA). J Neurol. 2023;270(5):2531–2546. doi:10.1007/s00415-023-11560-1.
50.
Crawford TO, Darras BT, Day JW, et al. Safety and Efficacy of Apitegromab in Patients With Spinal Muscular Atrophy Types 2 and 3: The Phase 2 TOPAZ Study. Neurology. 2024;102(5):e209151. doi:10.1212/WNL.0000000000209151.
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.