RESEARCH PAPER
Use of the ‘cuidando do pé’ app for risk classification and orientation regarding diabetic foot
1
Centro Universitario Lusíada, Santos, Brazil
2
Universidade Estadual do Oeste do Paraná, Cascaval, Brazil
Corresponding author
Gladson Ricardo Flor Bertolini
Universidade Estadual do Oeste do Paraná, Rua Universitária, 2069, 85819110, Cascavel, Brazil
Universidade Estadual do Oeste do Paraná, Rua Universitária, 2069, 85819110, Cascavel, Brazil
J Pre Clin Clin Res. 2023;17(2):47-51
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Diabetic foot is a complication of diabetes mellitus (DM) and is the leading cause of lower limb amputation. Use of the application ‘Cuidando do Pé’ (Caring for the Foot), with the aim of achieving better preventive alternatives and seeking better patient monitoring.
Material and methods:
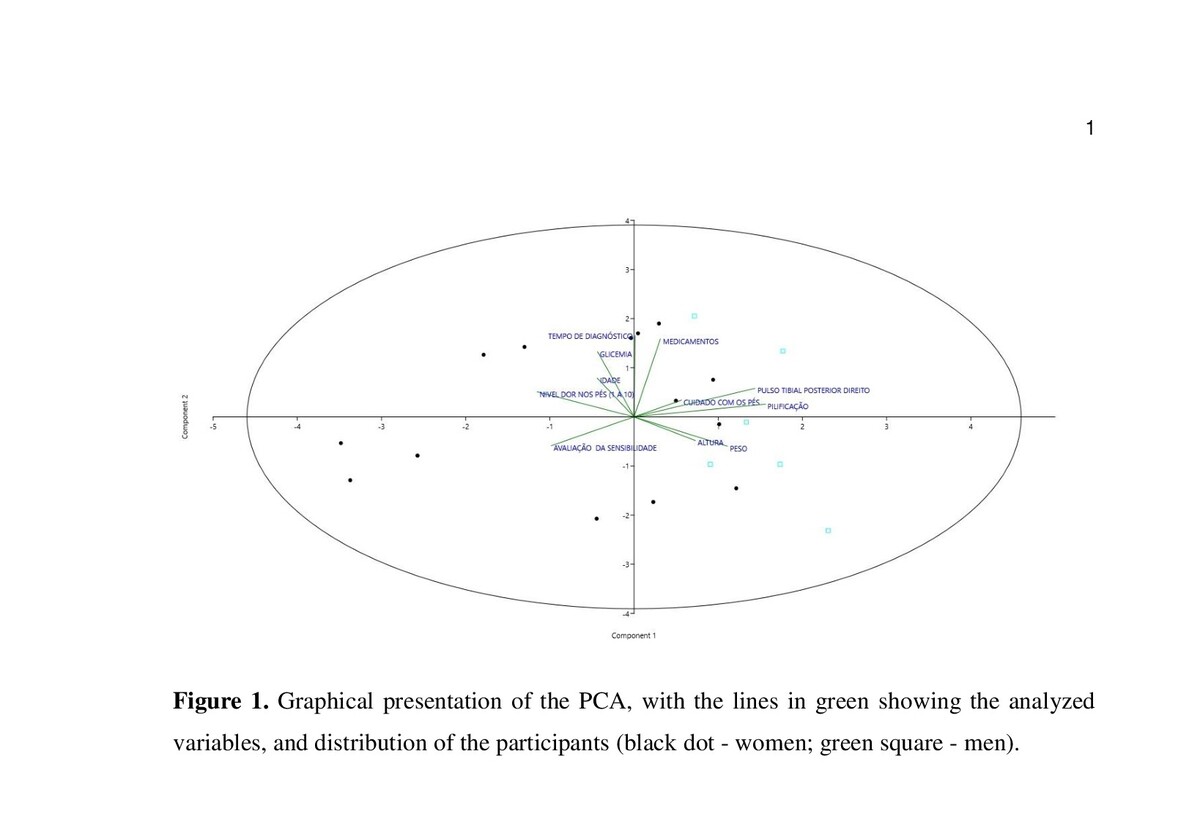
Cross-sectional study, carried out with 20 patients with Type II Diabetes Mellitus, in routine consultations between June – November 2022. The collection was performed from a questionnaire made available through the application ‘Cuidando do Pé’ and the behaviours given accordingly.
Results:
40% did not know about foot care; among those who did, 80% had never had their feet evaluated by health professionals, 55% did not perform proper care, and 30% claimed to have chronic pain at the site. None of the patients presented deformities or changes in skin integrity or colour; however, absent pilification (20%), xeroderma (25%), cracks (5%), hypertrophic (5%) or hypotrophic (5%) nails, humid (5%) or macerated (5%) interdigital spaces, decreased superficial (35%) and deep (5%) sensibility, altered reflexes (20%), lower limb oedema (15%), cold temperature (5%), and decreased peripheral pulses (up to 25%) were presented.
Conclusions:
Most of the patients with type II DM analysed did not perform proper foot care, and many did not know what this care was and were classified, on average, as having moderate risk of developing complications. Several alterations were presented, most of which could be avoided with routine consultations and more information on comorbidities associated with type II DM. The application ‘Cuidando do Pé’ is a viable alternative for better standardisation of care, also having simplicity and accessibility for health workers.
Diabetic foot is a complication of diabetes mellitus (DM) and is the leading cause of lower limb amputation. Use of the application ‘Cuidando do Pé’ (Caring for the Foot), with the aim of achieving better preventive alternatives and seeking better patient monitoring.
Material and methods:
Cross-sectional study, carried out with 20 patients with Type II Diabetes Mellitus, in routine consultations between June – November 2022. The collection was performed from a questionnaire made available through the application ‘Cuidando do Pé’ and the behaviours given accordingly.
Results:
40% did not know about foot care; among those who did, 80% had never had their feet evaluated by health professionals, 55% did not perform proper care, and 30% claimed to have chronic pain at the site. None of the patients presented deformities or changes in skin integrity or colour; however, absent pilification (20%), xeroderma (25%), cracks (5%), hypertrophic (5%) or hypotrophic (5%) nails, humid (5%) or macerated (5%) interdigital spaces, decreased superficial (35%) and deep (5%) sensibility, altered reflexes (20%), lower limb oedema (15%), cold temperature (5%), and decreased peripheral pulses (up to 25%) were presented.
Conclusions:
Most of the patients with type II DM analysed did not perform proper foot care, and many did not know what this care was and were classified, on average, as having moderate risk of developing complications. Several alterations were presented, most of which could be avoided with routine consultations and more information on comorbidities associated with type II DM. The application ‘Cuidando do Pé’ is a viable alternative for better standardisation of care, also having simplicity and accessibility for health workers.
Espinola A, Vinagreiro JR, Artioli DP, Bertolini GRF, Azevedo MVGT. Use of the ‘cuidando do pé’ app for risk classification and orientation
regarding diabetic foot. J Pre-Clin Clin Res. 2023; 17(2): 47–51. doi: 10.26444/jpccr/166117
REFERENCES (22)
1.
Shah SZA, Karam JA, Zeb A, et al. Movement is improvement: The therapeutic effects of exercise and general physical activity on glycemic control in patients with type 2 diabetes mellitus: A systematic review and meta-analysis of randomized controlled trials. Diabetes Therapy. 2021;12:707–732. https://doi.org/10.1007/s13300....
2.
Petersmann A, Müller-Wieland D, Müller UA, et al. Definition, classification and diagnosis of diabetes mellitus. Exp Clin Endocrinol Diabetes. 2019; 127:S1–S7. https://doi.org/10.1055/a-1018....
3.
Szmuilowicz ED, Josefson JL, Metzger BE. Gestational diabetes mellitus. Endocrinol Metab Clin North Am. 2019;48:479–493. https://doi.org/10.1016/j.ecl.....
4.
WHO – World Health Organization Health topics: Diabetes. In: https://www.who.int/news-room/.... https://www.who.int/news-room/.... Accessed 26 Feb 2023.
5.
Glovaci D, Fan W, Wong ND. Epidemiology of diabetes mellitus and cardiovascular disease. Curr Cardiol Rep. 2019;21:21. https://doi.org/10.1007/s11886....
6.
Gao S, Zhang H, Long C, Xing Z. Association between obesity and microvascular diseases in patients with type 2 diabetes mellitus. Front Endocrinol (Lausanne). 2021;12:7195151. https://doi.org/10.3389/fendo.....
7.
Mishra SC, Chhatbar KC, Kashikar A, Mehndiratta A. Diabetic foot. BMJ. 2017; Suppl 1:359. https://doi.org/10.1136/bmj.j5....
8.
Jeffcoate WJ. Charcot foot syndrome. Diabetic Med. 2015;32:760–770. https://doi.org/10.1111/dme.12....
9.
Singh N, Armstrong DG, Lipsky BA. Preventing foot ulcers in patients with diabetes. JAMA. 2005;293:217–228.
10.
Ramsey SD, Newton K, Blough D, et al. Incidence, outcomes, and cost of foot ulcers in patients with diabetes. Diabetes Care. 1999;22:382–387.
11.
Muro ES, Muro ID de O, Chaves E de CL, et al. Desenvolvimento e validação de um aplicativo para o exame dos pés da pessoa com diabetes mellitus. Revista UNILUS Ensino e Pesquisa. 2020;17:173–184.
12.
Tong SF, Low WY. Public health strategies to address Asian men’s health needs. Asia Pac J Public Health. 2012;24:543–555. https://doi.org/10.1177/101053....
13.
de Lima LJL, Lopes MR, Filho CA de LB, Cecon RS. Evaluation of self-care with feet among patients with diabetes mellitus. J Vasc Bras. 2022;21:e2021001. https://doi.org/10.1590/1677-5....
14.
Onianwa P, Ayorinde M, Akanbi F, et al. Outcome of an educational training programme on blood glucose monitoring among nurses in the management of hypoglycaemia and hyperglycemia. J Pre-Clin Clin Res. 2021;15:20–25. https://doi.org/10.26444/jpccr....
15.
Lemamsha H, Randhawa G, Papadopoulos C. Prevalence of overweight and obesity among Libyan men and women. Biomed Res Int. 2019:8531360. https://doi.org/10.1155/2019/8....
16.
Cooper AJ, Gupta SR, Moustafa AF, Chao AM. Sex/gender differences in obesity prevalence, comorbidities, and treatment. Curr Obes Rep. 2021;10:458–466. https://doi.org/10.1007/s13679....
17.
Bhupathiraju SN, Hu FB. Epidemiology of obesity and diabetes and their cardiovascular complications. Circ Res. 2016;118:1723–1735. https://doi.org/10.1161/CIRCRE....
18.
Lause M, Kamboj A, Faith EF. Dermatologic manifestations of endocrine disorders. Transl Pediatr. 2017;6:300–312. https://doi.org/10.21037/tp.20....
19.
Seyedizadeh SH, Cheragh-Birjandi S, Hamedi Nia MR. The effects of combined exercise training (resistance-aerobic) on serum kinesin and physical function in type 2 diabetes patients with diabetic peripheral neuropathy (randomized controlled trials). J Diabetes Res. 2020:6978128. https://doi.org/10.1155/2020/6....
20.
Dal Canto E, Ceriello A, Rydén L, et al. Diabetes as a cardiovascular risk factor: An overview of global trends of macro and micro vascular complications. Eur J Prev Cardiol. 2019;26:25–32. https://doi.org/10.1177/204748....
21.
Kumar MS, Lohiya A, Ramesh V, et al. Sensitivity and specificity of pulse oximetry and ankle-brachial index for screening asymptomatic peripheral vascular diseases in type 2 diabetes mellitus. J Assoc Physic India. 2016;64:38–43.
22.
Pititto B, Dias M, Moura F, Lamounier R, Calliari S, Bertoluci M. Metas no tratamento do diabetes. Diretriz Oficial da Sociedade Brasileira de Diabetes; 2022. doi: 10.29327/557753.2022-3, ISBN: 978-65-5941-622-6.