REVIEW PAPER
Tooth agenesis: genes and syndromic diseases –literature review
1
Scientific Circle at the Department of Paediatric Dentistry, University of Medical Science, Poznań, Poland
2
University of Medical Sciences, Poznan, Poland
Corresponding author
J Pre Clin Clin Res. 2022;16(4):149-152
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Tooth agenesis may be present even in 9.6% of individuals of both genders, with the predominance in permanent dentition. The aim of the study was to present a review of the literature on the etiology of dental agenesis, with particular emphasis on the genetic background and the associated syndromes of congenital abnormalities
Review methods:
Online databases were searched: Pubmed, GoogleScholar and Scopus. 32 articles from the last 18 years were qualified for the study and used in this review. Inclusion criteria were: children, congenital disorders, syndromic diseases, missing teeth, tooth agenesis. The study takes into account both syndromes common in the population and rare disorders.
Abbreviated description of the state of knowledge:
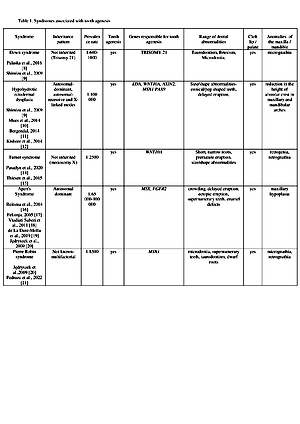
Many genes are responsible for both isolated and syndromic tooth agenesis. The most studied and involved in the formation of this anomaly are: MSX1, PAX9, AXIN2, WNT10A, EDA, TGF, SHH. The presented study shows that various forms of agenesis are caused by genes that involve interacting molecular pathways. The course of this phenomenon is very diverse, especially in syndromes of defects accompanied by other craniofacial anomalies.
Summary:
The absence of one or several teeth seriously disrupts the proper development of a child, as tooth agenesis affects the craniofacial development and psychosomatic development of a patient at developmental age. Children diagnosed withmissing tooth buds should receive comprehensive treatment, which includes dentists with such specialties as: maxillofacial surgeon, dental surgeon, orthodontist or prosthodontist.
Tooth agenesis may be present even in 9.6% of individuals of both genders, with the predominance in permanent dentition. The aim of the study was to present a review of the literature on the etiology of dental agenesis, with particular emphasis on the genetic background and the associated syndromes of congenital abnormalities
Review methods:
Online databases were searched: Pubmed, GoogleScholar and Scopus. 32 articles from the last 18 years were qualified for the study and used in this review. Inclusion criteria were: children, congenital disorders, syndromic diseases, missing teeth, tooth agenesis. The study takes into account both syndromes common in the population and rare disorders.
Abbreviated description of the state of knowledge:
Many genes are responsible for both isolated and syndromic tooth agenesis. The most studied and involved in the formation of this anomaly are: MSX1, PAX9, AXIN2, WNT10A, EDA, TGF, SHH. The presented study shows that various forms of agenesis are caused by genes that involve interacting molecular pathways. The course of this phenomenon is very diverse, especially in syndromes of defects accompanied by other craniofacial anomalies.
Summary:
The absence of one or several teeth seriously disrupts the proper development of a child, as tooth agenesis affects the craniofacial development and psychosomatic development of a patient at developmental age. Children diagnosed withmissing tooth buds should receive comprehensive treatment, which includes dentists with such specialties as: maxillofacial surgeon, dental surgeon, orthodontist or prosthodontist.
Klupś D, Kaźmierczak J, Torlińska-Walkowiak N. Tooth agenes: genes and syndromic diseases – literature review. J Pre-Clin Clin Res. 2022;
16(4): 149–152. doi: 10.26444/jpccr/157097
REFERENCES (32)
1.
Yu M, Wong SW, Han D, Cai T. Genetic analysis: Wnt and other pathways in nonsyndromic tooth agenesis. Oral Dis. 2019;25(3):646–651. https://doi.org/10.1111/odi.12....
2.
Bergendal B, Norderyd J, Zhou X, Klar J, Dahl N. Abnormal primary and permanent dentitions with ectodermal symptoms predict WNT10A deficiency. BMC Med Genet. 2016;17(1):88. https://doi.org/10.1186/ s12881-016-0349-4.
3.
Abu-Hussein M, Watted N, Yehia M. Clinical Genetic Basis of Tooth Agenesis. IOSR-JDMS. 2015;PP 68–77. https://doi.org/10.9790/0853-1....
4.
Rausch-Fan X, Özdemir B, Čelar A. Tooth Agenesis – CurrentPerspective of Recent Genetics and Clinical Implications. Informationen aus Orthodontie & Kieferorthopädie. 2014;46(01):3–7. https://doi. org/10.1055/s-0034-1371809.
5.
Kusiak A, Kochańska B, Bukowska M, et al. Hypodontia in maxillary permanent dentition – case report. Czas. Stomatol. 2008;61:348–352.
6.
Fournier BP, Bruneau MH, Toupenay S, et al. Patterns of Dental Agenesis Highlight the Nature of the Causative Mutated Genes. J Dent Res. 2018; 97(12):1306–1316. https://doi.org/10.1177/002203....
7.
Ye X, Attaie AB. Genetic Basis of Nonsyndromic and Syndromic Tooth Agenesis. J Pediatr Genet. 2016;5(4):198–208. https://doi. org/10.1055/s-0036-1592421.
8.
Palaska P, Antonarakis AG. Prevalence and patterns of permanent tooth agenesis in individuals with Down syndrome: a meta-analysis. Eur J Oral Sci. 2016;124(4):317–28. doi: https://doi.org/10.1111/eos.12....
9.
Shimizu T, Maeda T. Prevalence and genetic basis of tooth agenesis. Japanese Dent Scien Review. 2009;45(1):52–58.
10.
Mues G, Bonds J, Xiang L, et al. The WNT10A gene in ectodermal dysplasias and selective tooth agenesis. Am J Med Genet A. 2014; 164A(10):2455–60. https://doi.org/10.1002/ajmg.a....
11.
Bergendal B. Orodental manifestations in ectodermal dysplasia-a review. Am J Med Genet A. 2014;164(10):2465–71. https://doi.org/10.1002/ ajmg.a.36571.
12.
Kishore M, Panat SR, Aggarwal A, et al. Hypohidrotic Ectodermal Dysplasia (ED): A Case Series. J Clin Diagn Res. 2014;8(1):273–5. https:// doi.org/10.7860/JCDR/2014/6597.3951.
13.
Ahiko N, Baba Y, Tsuji M, et al. Investigation of maxillofacial morphology and dental development in hemifacial microsomia. Cleft Palate Craniofac J. 2015;52(2):203–9. https://doi.org/10.1111/cga.12....
14.
Pasadyn S, Haseley A, Irfan M. WNT10A Mutation Causes Ectodermal Dysplasia in a Patient Mosaic for Turner Syndrome. J Clin Aesthet Dermatol. 2020;13(6):57–58.
15.
Thiesen G, Ilha MC, Borges TS, et al. Turner syndrome case report: A multidisciplinary approach. Stomatos. 2015;21(40):12–20.
16.
Reitsma JH, Ongkosuwito EM, Arjen J, Wijk V, Prahl-Andersen B. Patterns of Tooth Agenesis in Patients with Crouzon or Apert Syndrome. Am J The Cleft Palate-Craniofacial. 2014;51(2):178–83. doi: https://doi. org/10.1597/12-180.
17.
Fekonja A. Hypodontia in orthodontically treated children. Eur J Orthod. 2005;27(5):457–60. https://doi.org/10.1093/ejo/cj....
18.
Vadiati Saberi B, Shakoorpour A. Apert Syndrome: Report of a Case with Emphasis on Oral Manifestations. J Den (Teheran). 2011;8(2):90–95.
19.
de La Dure-Molla M, Fournier BP, Manzanares MC. Elements of morphology: Standard terminology for the teeth and classifying genetic dental disorders. Am J Med Genet A. 2019;179(10):1913–1981. https:// doi.org/10.1002/ajmg.a.61316.
20.
Jędryszek A, Kmiecik M, Paszkiewicz A. Review of Modern Knowledge on Hypodontia. Dent Med Probl. 2009;46(1):118–125.
21.
Pedraza Deutsch E, Romero CC, Martinez Gonzales GI, et al. Pierre Robin syndrome, an update from a stomatological point of view. Int J Appl Dent Sci. 2022;8(2):182–185. https://doi.org/10.22271/oral..... v8.i2c.1508.
22.
Antonarakis GS, Suri S. Prevalence and patterns of permanent tooth agenesis in patients with nonsyndromic Pierre Robin sequence. Am J Orthod Dentofacial Orthop. 2014;145(4):452–60. doi: https://doi. org/10.1016/j.ajodo.2013.11.021.
23.
Houssaye G, Bieche I, Roche I, et al. Identification of the first intragenic deletion of the PITX2 gene causing an Axenfeld-Rieger Syndrome: case report. BMC Med Genet. 2006;7:82. https://doi.org/10.1186/1471- 2350-7-82.
24.
Fan Z, Sun S, Liu H, et al. Novel PITX2 mutations identified in Axenfeld- Rieger syndrome and the pattern of PITX2-related tooth agenesis. Oral Diseases. 2019;25(8):2010–2019. https://doi.org/10.1111/odi.13....
25.
Friebe-Hoffmann U, Reister F, Gaspar H. Das Wolf-Hirschhorn Syndrom. Z Geburtshilfe Neonatol. 2016;220(5):195–199. https://doi. org/10.1055/s-0042-107084.
26.
Pingul MM, Quintos JB. Van der woude syndrome (lip pit-cleft lip syndrome). J Pediatr. 2014;164(5):1235. https://doi.org/10.1016/j. jpeds.2013.12.039.
27.
Deshmukh PK, Deshmukh K, Mangalgi A, et al. Van der woude syndrome with short review of the literature. Case Rep Dent. 2014; 2014:871460. https://doi.org/10.1155/2014/8....
28.
Bohring A, Stamm T, Spaich C, et al. WNT10A mutations are a frequent cause of a broad spectrum of ectodermal dysplasias with sex-biased manifestation pattern in heterozygotes. Am J Hum Genet. 2009;85(1): 97–105. https://doi.org/10.1016/j.ajhg....
29.
Lugassy J, Itin P, Ishida-Yamamoto A, et al. Naegeli-Franceschetti- Jadassohn syndrome and dermatopathia pigmentosa reticularis: two allelic ectodermal dysplasias caused by dominant mutations in KRT14. Am J Hum Genet. 2006;79(4):724–30. https://doi.org/10.1086/507792.
30.
Goswami M, Chaitra TR, Singh S, et al. Congenitally missing primary mandibular lateral incisors: a case of rare occurrence. BMJ Case Rep. 2012; 2012: bcr2012006472. https://doi.org/10.1136/bcr-20....
31.
Tong HJ, Tahmassebi JF. Management of a child with severe hypodontia in the mixed dentition stage of development. Eur Arch Paediatr Dent. 2014;15(6):449–54. https://doi.org/10.1007/s40368....
32.
Kotecha S, Turner PJ, Dietrich T, et al. The impact of tooth agenesis on oral health-related quality of life in children. J Orthod. 2013;40(2): 122–9. https://doi.org/10.1179/146531....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.