REVIEW PAPER
The impact of piercing on various aspects of oral health
1
Student Research Group, Department of Oral Medicine, Medical University, Lublin, Poland
2
Department of Oral Medicine, Medical University of Lublin, Poland
Corresponding author
Alicja Srebrna
Student Research Group, Department of Oral Medicine, Medical University of Lublin, Poland, Doktora Witolda Chodźki 6, 20-093, Lublin, Poland
Student Research Group, Department of Oral Medicine, Medical University of Lublin, Poland, Doktora Witolda Chodźki 6, 20-093, Lublin, Poland
J Pre Clin Clin Res. 2021;15(4):204-207
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
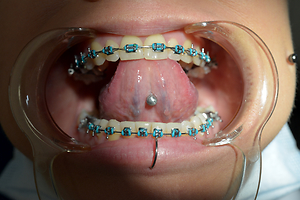
Oral piercing is especially popular among teenagers and young adults. It consists in piercing and placing decorative jewelry within the oral cavity, most often in the tongue and lips, and carries the risk of general and local complications – including dental and periodontal tissues, as well as oral mucosa. Because many people who decide to have oral piercing are not aware of this risk, this review aims to illustrate the multidimensionality and prevalence of complications occurring in people with oral piercing, the role of the dentist in educating and informing the patient about possible related complications the dangers it entails, as well as broadening knowledge and increasing the awareness of people considering piercing.
Review methods:
In order to accurately assess the risks associated with the use of piercings in the oral cavity, materials on the subject available on the PubMed platform were analyzed, and the most important issues and conclusions drawn were presented.
Brief description of the state of knowledge:
People with oral cavity piercings have worse hygiene than people without piercing, and have a higher risk of damage to the teeth and mucosa. Bacterial-related periodontal problems, such as deepening of periodontal pockets, loss of connective epithelium, and bleeding on probing, are also common. Lichenoid lesions and abnormalities in the histopathological examination may appear. In the case of metal earrings, galvanic current and corrosion are typical.
Summary:
Oral piercings can pose a risk to the health of the oral cavity and teeth. The role of the dentist is to treat and prevent complications by adopting a professional educational and preventive approach.
Oral piercing is especially popular among teenagers and young adults. It consists in piercing and placing decorative jewelry within the oral cavity, most often in the tongue and lips, and carries the risk of general and local complications – including dental and periodontal tissues, as well as oral mucosa. Because many people who decide to have oral piercing are not aware of this risk, this review aims to illustrate the multidimensionality and prevalence of complications occurring in people with oral piercing, the role of the dentist in educating and informing the patient about possible related complications the dangers it entails, as well as broadening knowledge and increasing the awareness of people considering piercing.
Review methods:
In order to accurately assess the risks associated with the use of piercings in the oral cavity, materials on the subject available on the PubMed platform were analyzed, and the most important issues and conclusions drawn were presented.
Brief description of the state of knowledge:
People with oral cavity piercings have worse hygiene than people without piercing, and have a higher risk of damage to the teeth and mucosa. Bacterial-related periodontal problems, such as deepening of periodontal pockets, loss of connective epithelium, and bleeding on probing, are also common. Lichenoid lesions and abnormalities in the histopathological examination may appear. In the case of metal earrings, galvanic current and corrosion are typical.
Summary:
Oral piercings can pose a risk to the health of the oral cavity and teeth. The role of the dentist is to treat and prevent complications by adopting a professional educational and preventive approach.
Srebrna A, Sutkowska P, Szwaj K, Puzio N, Szałkowska J, Strączek A, Thum-Tyzo K. The impact of piercing on various aspects of oral health.
J Pre-Clin Clin Res. 2021; 15(4): 204–207. doi: 10.26444/jpccr/145094
REFERENCES (15)
1.
Policy on Intraoral/Perioral Piercing and Oral Jewelry/Accessories. Pediatr Dent. 2016; 38(6): 74–75.
2.
Maspero C, Farronato G, Giannini L, Kairyte L, Pisani L, Galbiati G. The complication of oral piercing and the role of dentist in their prevention: a literature review. Stomatologija. 2014; 16(3): 118–24. https://doi.org/10.3390/ijerph....
3.
Inchingolo F, Tatullo M, Abenavoli FM, Marrelli M, Inchingolo AD, Palladino A, Inchingolo AM, Dipalma G. Oral piercing and oral diseases: a short time retrospective study. Int J Med Sci. 2011; 8(8): 649–52. https://dx.doi.org/10.7150%2Fi....
4.
Leichter JW, Monteith BD. Prevalence and risk of traumatic gingival recession following elective lip piercing. 2006; 22(1): 7–13. https://doi. org/10.1111/j.1600-9657.2006.00332.x.
5.
Domingo MG, Ferrari L, Aguas S, Alejandro FS, Steimetz T, Sebelli P, Olmedo DG. Oral exfoliative cytology and corrosion of metal piercings. Tissue implications. Clin Oral Investig. 2019; 23(4): 1895–1904. https:// doi.org/10.1007/s00784-018-2626-4.
6.
Farrukh F, Mânica S. Fashion for a reason: Oral jewellery to aid forensic odontology. J Forensic Leg Med. 2019; 66: 38–43. https://doi. org/10.1016/j.jflm.2019.06.002.
7.
Covello F, Salerno C, Giovannini V, Corridore D, Ottolenghi L, Vozza I. Piercing and Oral Health: A Study on the Knowledge of Risks and Complications. Int J Environ Res Public Health. 2020; 17(2): 613. https:// dx.doi.org/10.3390%2Fijerph17020613.
8.
Ziebolz D, Söder F, Hartl JF, Kottmann T, Rinke S, Merle CL, Schmalz G. Prevalence of periodontal pathogenic bacteria at different oral sites of patients with tongue piercing – results of a cross sectional study. Diagn Microbiol Infect Dis. 2019; 95(4): 114888. https://doi.org/10.1016/j. diagmicrobio.2019.114888.
9.
Schmidt JC, Calderaro S, Weiger R, Walter C. On the association between oral piercings and periodontal conditions-A case series. Int J Dent Hyg. 2019; 17(4): 318–326. https://doi.org/10.1111/idh.12....
10.
Hennequin-Hoenderdos NL, Slot DE, Van der Weijden GA. The incidence of complications associated with lip and/or tongue piercings:a systematic review. Int J Dent Hyg. 2016; 14(1): 62–73. https://doi. org/10.1111/idh.12118.
11.
Ziebolz D, Söder F, Hartl JF, Kottmann T, Rinke S, Schmalz G. Comprehensive assessment of dental behaviour and oral status in patients with tongue piercing-results of a cross-sectional study. Clin Oral Investig. 2020; 24(2): 971–977. https://doi.org/10.100 /s00784-019-03002-y.
12.
Stead LR, Williams JV, Williams AC, Robinson CM. An investigation into the practice of tongue piercing in the South West of England. Br Dent J. 2006; 200(2): 103–7. https://doi.org/10.1038/sj.bdj....
13.
Amadori F, Bardellini E, Conti G, Majorana A. Oral mucosal lesions in teenagers: a cross-sectional study. Italian Journal of Pediatrics. 2017; 43(1): 50 https://doi.org/10.1186/s13052....
14.
Preslar D, Borger J. Body Piercing Infections. In StatPearls. StatPearls Publishing; 2021.
15.
An J, Madeo J, Singhal M. Ludwig Angina. In StatPearls. StatPearls Publishing. 2021.
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.