CASE REPORT
Schmidt syndrome mimicking depression and refractory hypotension in critically ill patient – Case Report and Literature Review
1
Student Scientific Association, Second Department of Anesthesiology and Intensive Therapy, Medical University, Lublin, Poland
2
Second Department of Anesthesiology and Intensive Therapy, Medical University, Lublin, Poland
These authors had equal contribution to this work
Corresponding author
Joanna Chajec
Student Scientific Association, Second Department of Anesthesiology and Intensive Therapy, Medical University of Lublin, Poland
Student Scientific Association, Second Department of Anesthesiology and Intensive Therapy, Medical University of Lublin, Poland
J Pre Clin Clin Res. 2024;18(2):118-120
KEYWORDS
TOPICS
ABSTRACT
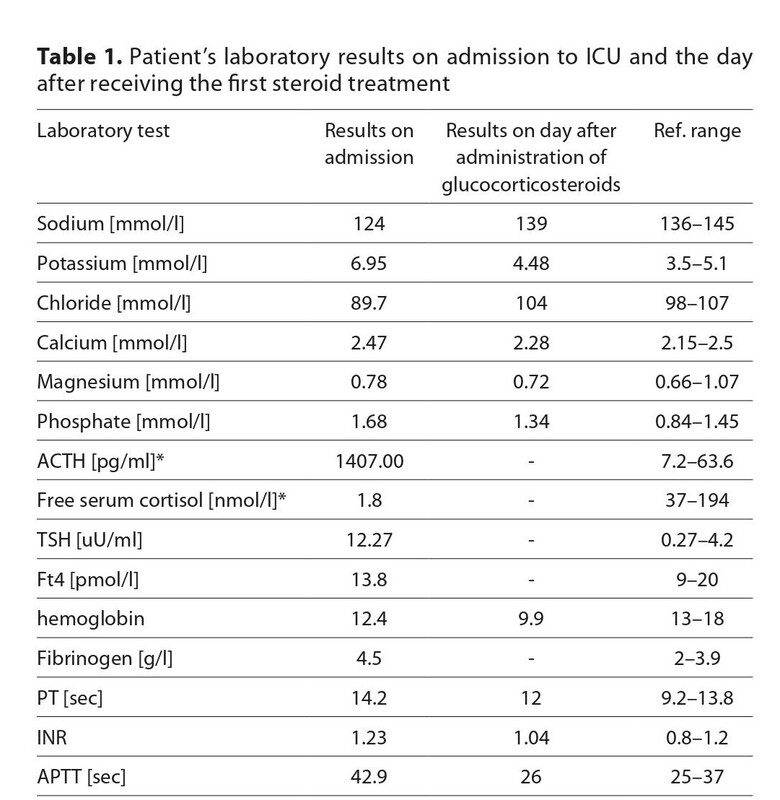
Schmidt syndrome is a disorder of the endocrine system associated with both autoimmune thyroid disease and primary
adrenal insufficiency. Nondistinctive nature and delayed appearance of the symptoms are difficult to diagnose. Moreover,
an untreated adrenal insufficiency crisis may lead to a life-threatening condition requiring rapid treatment, which includes
corticosteroids supplementation. We present a case of a 21-year-old male, with a history of thyroid disorder and depression,
who was admitted to the intensive care unit due to COVID-19 with circulatory insufficiency including persistent hypotension
and electrolyte imbalances. The patient was diagnosed with Schmidt syndrome and proper treatment was implemented.
Although Schmidt syndrome is a rare condition, appropriate diagnosis is a key to introducing proper treatment, which
despite being a lifetime commitment, can resolve all the symptoms.
FUNDING
Chajec J, Kutnik P. Schmidt syndrome mimicking depression and refractory hypotension in critically ill patient – case report and literature
review. J Pre-Clin Clin Res. 2023; 18(2): 118–120. doi: 10.26444/jpccr/187193
REFERENCES (21)
1.
Ten S, New M, Maclaren N. Addison’s disease 2001. J Clin Endocrinol Metabol. 2001;86(7):2909–2922. https://doi.org/10.1210 jcem.86.7.7636.
2.
Cutolo M. Autoimmune polyendocrine syndromes. Autoimmunity reviews. 2014;13(2): 85–89. https://doi.org/10.1016/j.autr....
3.
Chovel-Sella A, Halper A. Adrenal Insufficiency. Endocrine Conditions in Pediatrics. 2021: 285–288. https://doi.org/10.1007/978–3–....
5.
Wang X, Ping F, Qi C, Xiao X. Delayed diagnosis with autoimmune polyglandular syndrome type 2 causing acute adrenal crisis. Medicine (Balitmore). 2016;95(42): e5062. doi: 10.1097/MD.0000000000005062.
6.
Michels A, Michels N. Addison disease: early detection and treatment principles. Am Fam Physician. 2014;89(7): 563–568.
7.
Conrad N, Misra S, Verbakel JY, et al. Incidence, prevalence, and cooccurrence of autoimmune disorders over time and by age, sex, and socioeconomic status: a population-based cohort study of 22 million individuals in the UK. Lancet. 2023;401(10391):1878–1890. https://doi. org/10.1016/S0140–6736(23)00457–9.
8.
Meling Stokland AE, Ueland G, Lima K, et al. Autoimmune thyroid disorders in autoimmune Addison disease. J Clin Endocrinol Metab. 2022;107(6): e2331-e2338. https://doi.org/10.1210/clinem....
9.
Dalin F, Nordling Eriksson G, Dahlqvist P, et al. Clinical and immunological characteristics of autoimmune Addison disease: a nationwide Swedish multicenter study. J Clin Endocrinol Metab. 2017;102(2): 379–389. https://doi.org/10.1210/jc.201....
10.
Betterle C, Scarpa R, Garelli S, et al. Addison’s disease: a survey on 633 patients in Padova. Eur J Endocrinol. 2013;169(6): 773–784. https://doi. org/10.1530/EJE-13–0528.
11.
Heidari Z, Hajbagheri A. Assessment of serum cortisol and thyrotropin correlation in euthyroid and subclinical hypothyroid subjects. Exp Rev Endocrinol Metabol. 2021;16(5): 263–269. https://doi.org/10.1080/174466....
12.
Spoel E, Roelfsema F, Heemst D. Within-person variation in serum thyrotropin concentrations: main sources, pontential underlyingbiological mechanisms, and clinical implications. Front Endocrinol. 2021;12:619568. https://doi.org/10.3389/fendo.....
13.
Munawar M, Iftikhar PM, Hasan CA, et al. Neuropsychiatric manifestiation of Addison’s disease: a rare case report. Cureus. 2019;11(4):e4356. doi:10.7759/cureus.4356.
14.
Sanat ZM, Mohajeri-Tehrani MR. Psychotic disorder as the first manifestation of Addison Disease: a case report. Int J Endocrinol Metab. 2022;20(1);e121011. https://doi.org/10.5812/ijem.1....
15.
Lousada LM, Mendonca BB, Bachega TA SS. Adrenal crisis and mortality rate in adrenal insufficiency and congenital adrenal hyperplasia. Arch Endocrinol Metab. 2021;65(4):488–494. https://doi.org/10.20945/2359– 3997000000392.
16.
Cojocaru M, Cojocaru I M, Silosi I. Multiple autoimmune syndrome. Maedica. 2010;5(2):132–134.
17.
Moshynskyy A, Ho KH, Caspar-Bell G. A Case of Autoimmune Polyglandular Syndrome Type 2 Presenting as Dyspnea. Can Journ Gen Int Med. 2021;16(4):13–6. https://doi.org/10.22374/cjgim....
18.
Berta E, Lengyel I, Halmi S, et al. Hypertension in Thyroid Disorders. Front Endocrinol (Lausanne). 2019;10:482. doi: 10.3389/ fendo.2019.00482.
19.
Alexandraki K I, Sanpawithkayakul K, Grossman A. Adrenal Insufficiency. Endotext. 2022.
20.
Bhattarai, P, Allen H, Aggarwal A, Madden D, Dalton K. Unmasking of Addison’s disease in COVID-19. SAGE Open Medical Case Reports, 2021; 9: 2050313X211027758.
21.
Beshay L, Wei K, Yang Q. Newly diagnosed autoimmune Addison’s disease in a patient with COVID-19 with autoimmune disseminated encephalomyelitis. BMJ Case Reports. 2022; 15(12): e250749. https:// doi.org/10.1136/bcr-2022–250749.
Share
RELATED ARTICLE