REVIEW PAPER
Psychiatric disorders in women with polycystic ovary syndrome
1
Department of General Surgery, Stefan Kardynał Wyszyński Province Specialist Hospital, Lublin, Poland
2
Faculty of Medicine, Medical University, Lublin, Poland
3
Orthopedics and Rehabilitation Clinic, University Clinical Hospital No.4, Lublin, Poland
4
Clinical Department of Toxicology, Cardiology and Internal Diseases, Stefan Kardynał Wyszyński Province Specialist Hospital, Lublin, Poland
5
II Department of General Surgery, Gastroenterology and Digestive System Cancer, University Clinical Hospital No.1, Lublin, Poland
6
Paediatric Department, Independent Public Health Care Centre, Wyszków, Poland
7
Clinical Department of Cardiac Surgery, University Clinical Hospital No.4, Lublin, Poland
These authors had equal contribution to this work
Corresponding author
Bernadeta Maliszewska
Department of General Surgery, Stefan Kardynał Wyszyński Province Specialist Hospital in Lublin, Kraśnicka 100 avenue, 20-718 Lublin, Poland
Department of General Surgery, Stefan Kardynał Wyszyński Province Specialist Hospital in Lublin, Kraśnicka 100 avenue, 20-718 Lublin, Poland
J Pre Clin Clin Res. 2024;18(3):286-292
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Polycystic ovary syndrome (PCOS) is one of the most common gynecological endocrine disorders affecting women in reproductive age. Hyperandrogenism, oligoovulation, and polycystic ovaries seen on ultrasonography are its defining features. Women affected by PCOS are more susceptible to diabetes and dyslipidemia, as well as mental problems. Regarding the connection between PCOS and mental health, there are presently a number of theories. The aim of this study is to present the current knowledge of psychiatric disorders in women with PCOS, focusing on pathophysiology, molecular etiology and treatment.
Review methods:
A comprehensive literature review was performed using the electronic databases: PubMed, and Google Scholar. Key words, such as: ‘PCOS’, ‘polycystic ovary syndrome’, ‘psychiatric’, ‘psychiatric disorders’ and various combinations of the above were used. The search was limited by the year 2010 for all keywords.
Brief description of the state of knowledge:
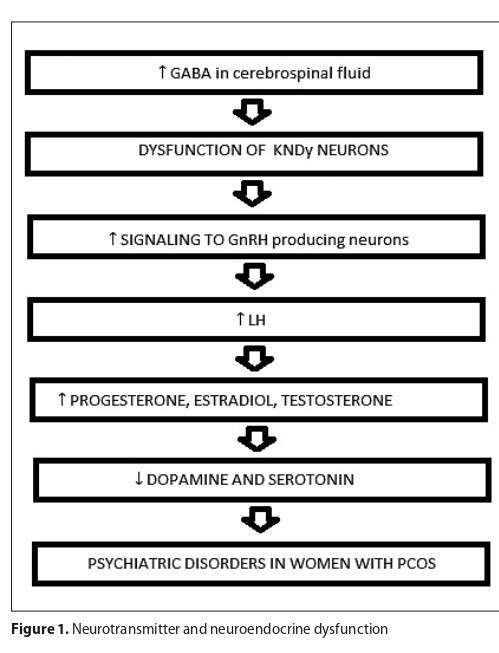
It is known that PCOS is linked to an increased prevalence of depression, bipolar disease, anxiety disorder and eating disorder. The literature review shows that the gut-brain axis, neurotransmitter and neuroendocrine dysfunction play significant roles in pathogenesis on the co occurrence of mental diseases and PCOS.
Summary:
Despite the potential socio-economic impact psychiatric disorders may have on PCOS patients and society, only a limited amount of research has been undertaken to investigate this relationship. The need for screening tests for all women with PCOS for mental disorders and adequately treat women diagnosed with these conditions is emphasized.
Polycystic ovary syndrome (PCOS) is one of the most common gynecological endocrine disorders affecting women in reproductive age. Hyperandrogenism, oligoovulation, and polycystic ovaries seen on ultrasonography are its defining features. Women affected by PCOS are more susceptible to diabetes and dyslipidemia, as well as mental problems. Regarding the connection between PCOS and mental health, there are presently a number of theories. The aim of this study is to present the current knowledge of psychiatric disorders in women with PCOS, focusing on pathophysiology, molecular etiology and treatment.
Review methods:
A comprehensive literature review was performed using the electronic databases: PubMed, and Google Scholar. Key words, such as: ‘PCOS’, ‘polycystic ovary syndrome’, ‘psychiatric’, ‘psychiatric disorders’ and various combinations of the above were used. The search was limited by the year 2010 for all keywords.
Brief description of the state of knowledge:
It is known that PCOS is linked to an increased prevalence of depression, bipolar disease, anxiety disorder and eating disorder. The literature review shows that the gut-brain axis, neurotransmitter and neuroendocrine dysfunction play significant roles in pathogenesis on the co occurrence of mental diseases and PCOS.
Summary:
Despite the potential socio-economic impact psychiatric disorders may have on PCOS patients and society, only a limited amount of research has been undertaken to investigate this relationship. The need for screening tests for all women with PCOS for mental disorders and adequately treat women diagnosed with these conditions is emphasized.
Maliszewska B, Tokarzewska A, Łasica M, Małyszek M, Łaba Ł, Dziurda S, Łomża-Łaba AW, Łuczyński D. Psychiatric disorders in women with
Polycystic Ovary Syndrome. J Pre-Clin Clin Res. 2024; 18(3): 286–292. doi: 10.26444/jpccr/192128
REFERENCES (41)
1.
Sadeghi HM, Adeli I, Calina D, et al. Polycystic Ovary Syndrome: A Comprehensive Review of Pathogenesis, Management, and Drug Repurposing. Int J Mol Sci. 2022 Jan6;23(2):583. https://doi.org/10.3390/ ijms23020583.
2.
Witchel SF, Oberfield SE, Peña AS. Polycystic Ovary Syndrome: Pathophysiology, Presentation, and Treatment With Emphasis on Adolescent Girls. J Endocr Soc. 2019 Jun 14;3(8):1545–1573. https:// doi.org/10.1210/js.2019-00078.
3.
Armanini D, Boscaro M, Bordin L, et al. Controversies in the Pathogenesis, Diagnosis and Treatment of PCOS: Focus on Insulin Resistance, Inflammation, and Hyperandrogenism. Int J Mol Sci. 2022 Apr 8;23(8):4110. https://doi.org/10.3390/ijms23....
4.
Siddiqui S, Mateen S, Ahmad R, et al. A brief insight into the etiology, genetics, and immunology of polycystic ovarian syndrome (PCOS). J Assist Reprod Genet. 2022 Nov;39(11):2439–2473. https://doi. org/10.1007/s10815-022-02625-7.
5.
Bulsara J, Patel P, Soni A, et al. A review: Brief insight into Polycystic Ovarian syndrome. Endocrine and Metabolic Science. 2021;3:100085. http://dx.doi.org/10.1016/j.en....
6.
Jabeen A, Yamini V, Rahman Amberina A, et al. Polycystic Ovarian Syndrome: Prevalence, Predisposing Factors, and Awareness Among Adolescent and Young Girls of South India. Cureus. 2022 Aug 12;14(8):e27943. https://doi.org/10.7759/cureus....
7.
Ajmal N, Khan SZ, Shaikh R. Polycystic ovary syndrome (PCOS) and genetic predisposition: A review article. Eur J Obstet Gynecol Reprod Biol X. 2019 Jun 8;3:100060. https://doi.org/10.1016/j.euro....
8.
Sarahian N, Sarvazad H, Sajadi E, et al. Investigation of common risk factors between polycystic ovary syndrome and Alzheimer’s disease: a narrative review. Reprod Health. 2021 Jul 26;18(1):156. https://doi. org/10.1186/s12978-021-01203-x.
9.
Rodriguez Paris V, Wong XYD, Solon-Biet SM, et al. The interplay between PCOS pathology and diet on gut microbiota in a mouse model. Gut Microbes. 2022 Jan-Dec;14(1):2085961. https://doi.org/10.1080% 2F19490976.2022.2085961.
10.
Dubey P, Reddy S, Boyd S, et al. Effect of Nutritional Supplementation on Oxidative Stress and Hormonal and Lipid Profiles in PCOSAffected Females. Nutrients. 2021 Aug 25;13(9):2938. https://doi. org/10.3390%2Fnu13092938.
11.
Deeks AA, Gibson-Helm ME, Paul E, et al. Is having polycystic ovary syndrome a predictor of poor psychological function including anxiety and depression? Hum Reprod. 2011 Jun;26(6):1399–407. https://doi. org/10.1093/humrep/der071.
12.
Dokras A, Clifton S, Futterweit W, et al. Increased risk for abnormal depression scores in women with polycystic ovary syndrome: a systematic review and meta-analysis. Obstet Gynecol. 2011 Jan;117(1):145–152. https://doi.org/10.1097/aog.0b....
13.
Rodriguez-Paris D, Remlinger-Molenda A, Kurzawa R, et al. Psychiatric disorders in women with polycystic ovary syndrome. Psychiatr Pol. 2019 Aug 31;53(4):955–966. English, Polish. https://doi.org/10.12740/ pp/onlinefirst/93105.
14.
Cesta CE, Månsson M, Palm C, et al. Polycystic ovary syndrome and psychiatric disorders: Co-morbidity and heritability in a nationwide Swedish cohort. Psychoneuroendocrinology. 2016Nov;73:196–203. https://doi.org/10.1016/j.psyn....
15.
Rassi A, Veras AB, dos Reis M, et al. Prevalence of psychiatric disorders in patients with polycystic ovary syndrome. Compr Psychiatry. 2010 Nov-Dec;51(6):599–602. https://doi.org/10.1016/j.comp....
16.
Doretto L, Mari FC, Chaves AC. Polycystic Ovary Syndrome and Psychotic Disorder. Front Psychiatry. 2020 Jun 10;11:543. https://doi. org/10.3389/fpsyt.2020.00543.
18.
Craske MG, Stein MB, Eley TC, et al. Anxiety disorders. Nat Rev Dis Primers. 2017 May 4;3:17024. https://doi.org/10.1038 nrdp.2017.24.
19.
Struijs SY, de Jong PJ, Jeronimus BF, et al. Psychological risk factors and the course of depression and anxiety disorders: A review of 15 years NESDA research. J Affect Disord. 2021 Dec 1;295:1347–1359. https:// doi.org/10.1016/j.jad.2021.08.086.
20.
Zimmermann M, Chong AK, Vechiu C, et al. Modifiable risk and protective factors for anxiety disorders among adults: A systematic review. Psychiatry Res. 2020 Mar;285:112705. https://doi.org/10.1016/j. psychres.2019.112705.
21.
Goodman WK, Grice DE, Lapidus KA, et al. Obsessive-compulsive disorder. PsychiatrClin North Am. 2014 Sep;37(3):257–67. https://doi. org/10.1016/j.psc.2014.06.004.
22.
Richter PMA, Ramos RT. Obsessive-Compulsive Disorder. Continuum (MinneapMinn). 2018 Jun;24(3, BEHAVIORAL NEUROLOGY AND PSYCHIATRY):828–844. https://doi.org/10.1212/ con.0000000000000603.
23.
Dybciak P, Raczkiewicz D, Humeniuk E, et al. Depression in PolycysticOvarySyndrome: A SystematicReview and Meta-Analysis. J Clin Med. 2023 Oct 10;12(20):6446. https://doi.org/10.3390/ medicina58070942.
24.
Fried EI, Epskamp S, Nesse RM, et al. What are ‘good’ depression symptoms? Comparing the centrality of DSM and non-DSM symptoms of depression in a network analysis. J Affect Disord. 2016 Jan 1;189:314–20. https://doi.org/10.1016/j.jad.....
25.
Grande I, Berk M, Birmaher B, et al. Bipolar disorder. Lancet. 2016 Apr 9;387(10027):1561–1572. https://doi.org/10.1016 s0140-6736(15)00241-x.
26.
Malhi GS, Berk M. Diagnosing bipolar disorder: Defining thresholds and setting boundaries. Aust N Z J Psychiatry. 2014 Jun;48(6):500–4. https://doi.org/10.1177/000486....
27.
McIntyre RS, Berk M, Brietzke E, et al. Bipolardisorders. Lancet. 2020 Dec 5;396(10265):1841–1856. https://doi.org/10.1016/s0140-....
28.
Yu Z, Muehleman V. Eating Disorders and Metabolic Diseases. Int J Environ Res Public Health. 2023 Jan 30;20(3):2446. https://doi. org/10.3390/ijerph20032446.
29.
Treasure J, Duarte TA, Schmidt U. Eating disorders. Lancet. 2020 Mar 14;395(10227):899–911. https://doi.org/10.1016/s0140-....
30.
Ilie IR. Neurotransmitter, neuropeptide and gut peptide profile in PCOS-pathways contributing to the pathophysiology, food intake and psychiatric manifestations of PCOS. Adv Clin Chem. 2020;96:85–135. https://doi.org/10.1016/bs.acc....
31.
Brutocao C, Zaiem F, Alsawas M, et al. Psychiatric disorders in women with polycystic ovary syndrome: a systematic review and meta-analysis. Endocrine. 2018 Nov;62(2):318–325. https://doi.org/10.1007/s12020....
32.
Steegers-Theunissen RPM, Wiegel RE, Jansen PW, et al. Polycystic Ovary Syndrome: A Brain Disorder Characterized by Eating Problems Originating during Puberty and Adolescence. Int J Mol Sci. 2020 Nov 3;21(21):8211. https://doi.org/10.3390/ijms21....
33.
Sarkisian KI, Ho L, Yang J, et al. Neuroendocrine, neurotransmitter, and gut microbiota imbalance contributing to potential psychiatric disorder prevalence in polycystic ovarian syndrome. F S Rep. 2023 Sep 9;4(4):337–342. https://doi.org/10.1016/j.xfre....
34.
Xing L, Xu J, Wei Y, et al. Depression in Polycystic Ovary Syndrome: Focusing on Pathogenesis and Treatment. Focus (Am Psychiatr Publ). 2024 Jan;22(1):109–119. https://doi.org/10.3389/fpsyt.....
35.
Dokras A. Mood and anxiety disorders in women with PCOS. Steroids. 2012 Mar10;77(4):338–41. https://doi.org/10.1016/j.ster....
36.
ZareMobini F, Kazemi A, Farajzadegan Z. A comprehensive mental health care program for women with polycystic ovary syndrome: protocol for a mixed methods study. Reprod Health. 2018 Mar 13;15(1):46. https://doi.org/10.1186/s12978....
37.
Palomba S, Santagni S, Falbo A, et al. Complications and challenges associated with polycystic ovary syndrome: current perspectives. Int J Womens Health. 2015 Jul 31;7:745–63. https://doi.org/10.2147/ijwh.s....
38.
Che Y, Yu J, Li YS, et al. Polycystic Ovary Syndrome: Challenges and Possible Solutions. J Clin Med. 2023 Feb 14;12(4):1500. https://doi.org/10.3390/jcm120....
39.
Banting LK, Gibson-Helm M, Polman R, et al. Physical activity and mental health in women with polycystic ovary syndrome. BMC Womens Health. 2014 Mar 27;14(1):51. https://doi.org/10.1186/1472-6....
40.
Kolhe JV, Chhipa AS, Butani S, et al. PCOS and Depression: Common Links and Potential Targets. Reprod Sci. 2022 Nov;29(11):3106–3123. https://doi.org/10.1007/s43032....
41.
Fauser BC, Tarlatzis BC, Rebar RW, et al. Consensus on women’s health aspects of polycystic ovary syndrome (PCOS): the Amsterdam ESHRE/ASRM-Sponsored 3rd PCOS Consensus Workshop Group. Fertil Steril. 2012 Jan;97(1):28–38.e25. https://doi.org/10.1016/j.fert....
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.