REVIEW PAPER
Paediatric inguinal hernia anatomical classifications – new perspectives for study design
1
Institute of Medical Sciences, University of Opole, Poland
J Pre Clin Clin Res. 2023;17(2):106-108
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Inguinal hernia is a common congenital surgical problem in children. There are many techniques for surgical treatment. Due to the fact that so many solutions exist to the problem of inguinal hernia in children, the best choice of surgical technique for a particular patient seems crucial. In the literature, there are many studies designed to compare the results of surgical treatment. It is probable that different types of hernia can be related to different results when a particular technique is used. The laparoscopic approach gives a new perspective to classifying paediatric inguinal hernia. The review aims to summarize the classification systems used in the description of paediatric inguinal hernias.
Review methods:
The review is based on academic literature and scientific publications available in PubMed and NCBI – National Library of Medicine databases. After evaluation of abstracts, articles were selected and analyzed, considering the references cited.
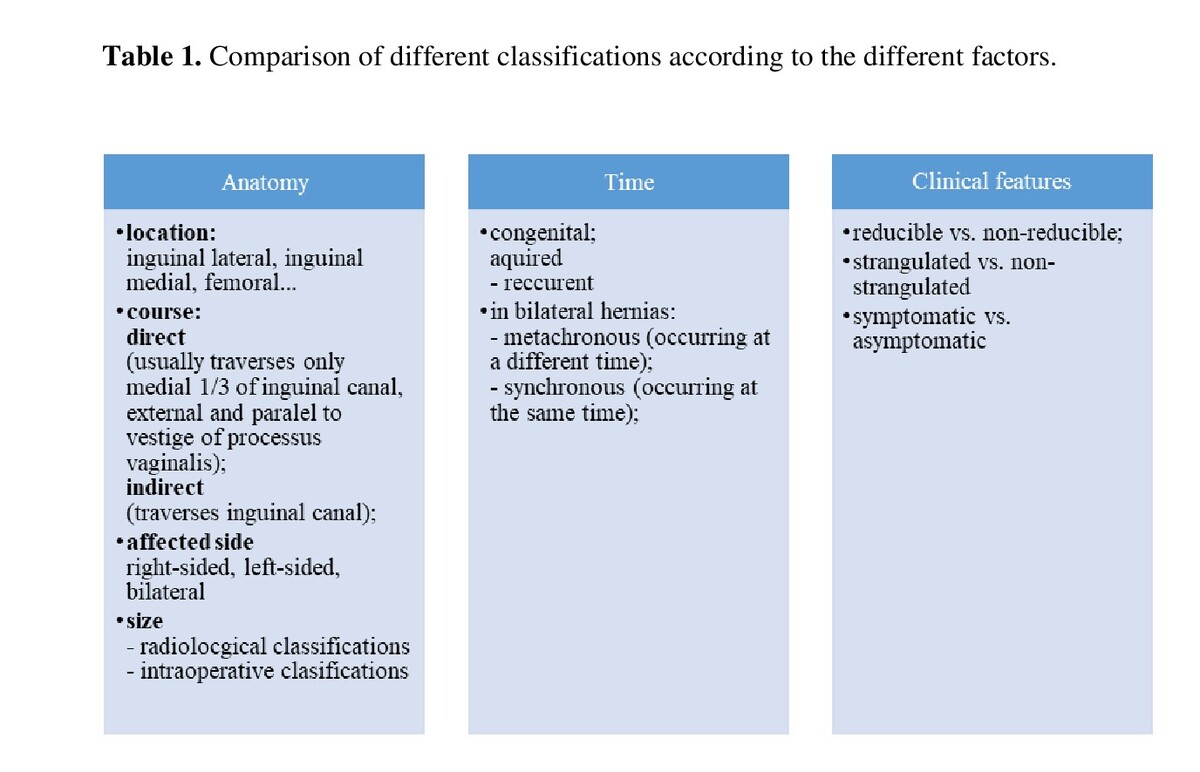
Brief description of the state of knowledge. Apart from classical anatomical classifications, the review indicates promising new classifications. Shehata et al. proposed a paediatric hernia classification and tailored treatment modified from the original Nyhus classification for adults, with suggested tailored treatment for each subtype. Toki et al. proposed the ultrasonographic classification for paediatric inguinal hernia. Tanaka et al. assessed the size of the hernia orifice during laparoscopy and used the classification by the European Hernia Society (EHS) for adult patients.
Summary:
A unified paediatric inguinal hernia classification would be useful not only for pre- or intra-operative descriptions of the anatomy and size of a hernia. The unification of the classification system of a paediatric inguinal hernia could also be helpful in the study design.
Inguinal hernia is a common congenital surgical problem in children. There are many techniques for surgical treatment. Due to the fact that so many solutions exist to the problem of inguinal hernia in children, the best choice of surgical technique for a particular patient seems crucial. In the literature, there are many studies designed to compare the results of surgical treatment. It is probable that different types of hernia can be related to different results when a particular technique is used. The laparoscopic approach gives a new perspective to classifying paediatric inguinal hernia. The review aims to summarize the classification systems used in the description of paediatric inguinal hernias.
Review methods:
The review is based on academic literature and scientific publications available in PubMed and NCBI – National Library of Medicine databases. After evaluation of abstracts, articles were selected and analyzed, considering the references cited.
Brief description of the state of knowledge. Apart from classical anatomical classifications, the review indicates promising new classifications. Shehata et al. proposed a paediatric hernia classification and tailored treatment modified from the original Nyhus classification for adults, with suggested tailored treatment for each subtype. Toki et al. proposed the ultrasonographic classification for paediatric inguinal hernia. Tanaka et al. assessed the size of the hernia orifice during laparoscopy and used the classification by the European Hernia Society (EHS) for adult patients.
Summary:
A unified paediatric inguinal hernia classification would be useful not only for pre- or intra-operative descriptions of the anatomy and size of a hernia. The unification of the classification system of a paediatric inguinal hernia could also be helpful in the study design.
Kawalec AM. Pediatric inguinal hernia anatomical classifications – new perspectives for study design. J Pre-Clin Clin Res. 2023; 17(2): 106–108. doi: 10.26444/jpccr/166130
REFERENCES (18)
1.
Morini F, Dreuning KMA, Janssen Lok MJH, et al. Surgical Management of Paediatric Inguinal Hernia: A Systematic Review and Guideline from the European Paediatric Surgeons’ Association Evidence and Guideline Committee. Eur J Pediatr Surg. 2022;32(3):219–232. https:// doi.org/10.1055/s-0040-1721420.
2.
Craner DR, Glenn IC, Ponsky TA. Inguinal Hernia Repair in Children. In: LaPinska MP, Blatnik JA, editors. Surgical Principles in Inguinal Hernia Repair. A Comprehensive Guide to Anatomy and Operative Techniques. Springer Nature: Switzerland; 2018. pp 139–147.
3.
Moore KL, Agur AMR, Dalley AF. Essential clinical anatomy. Wolters Kluwer: Philadelphia; 2019.
4.
Yeap E, Pacilli M, Nataraja RM. Inguinal hernias in children. Aust J Gen Pract. 2020;49(1–2):38–43. https://doi.org/10.31128/AJGP-....
5.
Lee SR. Laparoscopic iliopubic tract repair to treat recurrent paediatric inguinal hernia. Surgical Endoscopy. 2022;36(6):4321–4327. https://doi. org/10.1007/s00464-021-08776-5.
6.
HerniaSurge Group. International guidelines for groin hernia management. Hernia. 2018;22(1):1–165. https://doi.org/10.1007/s10029....
7.
Shehata S, Shehata S, Wella HL, et al. Paediatric inguinal hernias, are they all the same? A proposed paediatric hernia classification and tailored treatment. Hernia. 2018;22(6):941–946. doi:10.1007/s10029- 018-1816-y.
8.
Johnson KN, Criss CN, Hirschl RB, et al. ltrasound-guided paediatric inguinal hernia repair. J Pediatr Surg. 2021;56(7):1240–1245. doi:10.1016/j.jpedsurg.2021.02.053.
9.
Dreuning KMA, Ten Broeke CEM, Twisk JWR, et al. Diagnostic accuracy of preoperative ultrasonography in predicting contralateral inguinal hernia in children: a systematic review and meta-analysis. Eur Radiol. 2019;29(2):866–876. https://doi.org/10.1007/s00330....
10.
Brainwood M, Beirne G, Fenech M. Persistence of the processus vaginalis and its related disorders. Australas J Ultrasound Med. 2020;23(1):22–29. https://doi.org/10.1002/ajum.1....
11.
Yip PKF. Ultrasound detection and closure of contralateral patent processus vaginalis in paediatric patients with unilateral inguinal hernia and hydrocele: a longitudinal study to prove efficacy in avoiding contralateral hernia development. Hernia. 2019;23(6):1253–1259. https:// doi.org/10.1007/s10029-019-01951-7.
12.
Toki A, Ogura K, Miyauchi A. Ultrasonographic diagnosis of inguinal hernia in children. Pediatr Surg Int. 1995;10:541–543. https://doi. org/10.1007/BF00566492.
13.
Toki A, Watanabe Y, Sasaki K, et al. Ultrasonographic diagnosis for potential contralateral inguinal hernia in children. J Pediatr Surg. 2003;38:224–226. https://doi.org/10.1053/jpsu.2....
14.
Toki A, Watanabe Y, Sasaki K, et al. Adopt a wait-and-see attitude for patent processus vaginalis in neonates. J Pediatr Surg. 2003;38(9):1371–3. https://doi.org/10.1016/s0022-....
15.
Tanaka K, Watanobe I, Nakazawa-Tanaka N, et al. Assessment of laparoscopic inguinal hernia repair using the classification for single port laparoscopy in adolescents and young adults. Minerva Surg. 2022;5. https://doi.org/10.23736/S2724....
16.
Katoh R, Ogawa H, Takada T, et al. Significance of routine preoperative prone computed tomography for predicting intractable cases of inguinal hernias treated by transabdominal preperitoneal repair. Medicine (Baltimore). 2022;2;101(48):e31917. https://doi.org//10.1097/ MD.0000000000031917.
17.
Hosoda T, Hijikata K, Ishioka S. Rare case of inguinal ureteral hernia in a child diagnosed by drip infusion pyelography-computed tomography. Int J Surg Case Rep. 2022;94:107007. doi:10.1016/j.ijscr.2022.107007.
18.
Miserez M, Alexandre JH, Campanelli G, et al. The European hernia society groin hernia classification: simple and easy to remember. Hernia. 2007;11(2):113–6. https://doi.org/:10.1007/s1002....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.