RESEARCH PAPER
Oral epithelial dysplasia and oral cancer prevalence in routine white lesion biopsies – a 6-year retrospective study
1
Medical University, Łódź, Poland
J Pre Clin Clin Res. 2020;14(3):63-68
KEYWORDS
TOPICS
ABSTRACT
Introduction:
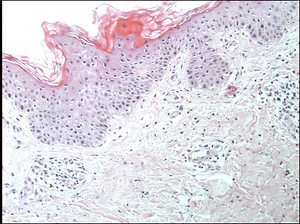
Leukoplakia and oral lichen planus (OLP) are common diseases manifesting as white lesions that are considered potentially malignant disorders (PMD). Epithelial dysplasia may be an early sign of potency for the future transformation into oral squamous cell carcinoma (OSCC). A routine biopsy and close observation are recommended for persistent white oral lesions. As frictional keratosis may mimic oral leukoplakia, the question arises:Is there a need for a biopsy of persistent white lesion of traumatic origin?
Material and methods:
Data from 643 oral tissue biopsies were retrospectively analyzed. A total of 176 (27.37%) results with provisional diagnosis of leukoplakia (36 cases), OLP (77 cases) and frictional keratosis (63 cases) were selected. Retrospective data collected included age, gender, smoking status, provisional and histopathological diagnosis. The data was analyzed to assess the prevalence of epithelial dysplasia and OSCC in terms of age, gender and smoking status.
Results:
Five (2.84%) cases of OSSC were reported, all of them were graded as G1; four cases of OSCC were found in clinically defined leukoplakia lesions; one case of OSCC (1.3%) was found in OLP biopsy; epithelial dysplasia was reported in 5 lesions (2.84%) provisionally diagnosed as OLP (3 cases), and leukoplakia in 2 cases. No dysplasia or OSCC were found in the lesions diagnosed as frictional keratosis.
Conclusions:
Epithelial dysplasia and OSCC may be found in leukoplakia or OLP lesions not initially suspected of any malignancy. In some cases, clinical features are not sufficient to diagnose a lesion without histopathology. Frictional keratosis is easily identified by clinicians, and may not require a biopsy in every case. Clinical and histopathological evaluation of the white lesions still needs improvement
Leukoplakia and oral lichen planus (OLP) are common diseases manifesting as white lesions that are considered potentially malignant disorders (PMD). Epithelial dysplasia may be an early sign of potency for the future transformation into oral squamous cell carcinoma (OSCC). A routine biopsy and close observation are recommended for persistent white oral lesions. As frictional keratosis may mimic oral leukoplakia, the question arises:Is there a need for a biopsy of persistent white lesion of traumatic origin?
Material and methods:
Data from 643 oral tissue biopsies were retrospectively analyzed. A total of 176 (27.37%) results with provisional diagnosis of leukoplakia (36 cases), OLP (77 cases) and frictional keratosis (63 cases) were selected. Retrospective data collected included age, gender, smoking status, provisional and histopathological diagnosis. The data was analyzed to assess the prevalence of epithelial dysplasia and OSCC in terms of age, gender and smoking status.
Results:
Five (2.84%) cases of OSSC were reported, all of them were graded as G1; four cases of OSCC were found in clinically defined leukoplakia lesions; one case of OSCC (1.3%) was found in OLP biopsy; epithelial dysplasia was reported in 5 lesions (2.84%) provisionally diagnosed as OLP (3 cases), and leukoplakia in 2 cases. No dysplasia or OSCC were found in the lesions diagnosed as frictional keratosis.
Conclusions:
Epithelial dysplasia and OSCC may be found in leukoplakia or OLP lesions not initially suspected of any malignancy. In some cases, clinical features are not sufficient to diagnose a lesion without histopathology. Frictional keratosis is easily identified by clinicians, and may not require a biopsy in every case. Clinical and histopathological evaluation of the white lesions still needs improvement
Kuzio M, Wapniarska K, Danilewicz M, Lewkowicz N. Oral epithelial dysplasia and oral cancer prevalence in routine white lesion biopsies –
a 6-year retrospective study. J Pre-Clin Clin Res. 2020; 14(3): 63–68. doi: 10.26444/jpccr/125393
REFERENCES (28)
1.
Warnakulasuriya S. Global epidemiology of oral and oropharyngeal cancer. Oral Oncol. 2009; 45: 309–316. https://doi.org/10.1016/j.oral....
2.
Müller S. Frictional Keratosis, Contact Keratosis and Smokeless Tobacco Keratosis: Features of Reactive White Lesions of the Oral Mucosa. Head Neck Pathol. 2019; 13(1): 16–24. https://doi.org/10.1007/s12105....
3.
Bánóczy J. Oral leukoplakia and other white lesions of the oral mucosa related to dermatological disorders. J Cutan Pathol. 1983; 10(4): 238–56. https://doi.org/10.1111/j.1600....
4.
Zaini ZM, McParland H, Møller H, Husband K, Odell EW. Predicting malignant progression in clinically high-risk lesions by DNA ploidy analysis and dysplasia grading. Sci Rep. 2018; 8(1): 15874. https://doi.org/10.1038/s41598....
5.
Cowan C, Gregg T, Napier S, McKenna S, Kee F. Potentially malignant oral lesions in Northern Ireland: a 20-year population-based perspective of malignant transformation. Oral Dis. 2001; 7(1): 18–24.
6.
Tilakaratne WM, Jayasooriya PR, Jayasuriya NS, De Silva RK. Oral epithelial dysplasia: Causes, quantification, prognosis, and management challenges. Periodontol 2000. 2019; 80(1): 126–147 https://doi.org /10.1111/prd.12259.
7.
van der Waal I. Oral leukoplakia, the ongoing discussion on definition and terminology. Med Oral Patol Oral Cir Bucal. 2015; 20(6): e685–92. https://doi.org/10.4317/medora....
8.
Axéll T. Occurrence of leukoplakia and some other oral white lesions among 20,333 adult Swedish people. Community Dent Oral Epidemiol. 1987; 15(1): 46–51. https://doi.org/10.1111/j.1600....
9.
Eisen D. The clinical features, malignant potential, and systemic associations of oral lichen planus: A study of 723 patients. J Am Acad Dermatol. 2002; 46(2): 207–14. https://doi.org/10.1067/mjd.20....
10.
Wagner G, Rose C, Sachse MM. Clinical variants of lichen planus. J Dtsch Dermatol Ges. 2013; 11(4): 309–19. https://doi.org/10.1111/ddg.12....
11.
Shirasuna K. Oral lichen planus: malignant potential and diagnosis. Oral Sci Int. 2014; 11: 1–7. https://doi.org/10.1016/S1348-....
12.
Mignogna MD1, Fortuna G, Leuci S, Adamo D, Siano M, Makary C, et al. Frictional keratoses on the facial attached gingiva are rare clinical findings and do not belong to the category of leukoplakia. J Oral Maxillofac Surg. 2011; 69(5): 1367–74. https://doi.org/10.1016/j.joms....
13.
Rad M, Hashemipoor MA, Mojtahedi A, Zarei MR, Chamani G, Kakoei S, et al. Correlation between clinical and histopathologic diagnoses of oral lichen planus based on modified WHO diagnostic criteria. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009; 107(6): 796–800 https://doi.org/10.1016/j.trip....
14.
Waldron CA, Shafer WG. Leukoplakia revisited. A clinicopathological study of 3256 oral leukoplakias. Cancer. 1975; 36(4): 1386–1392. https://doi.org/10.1002/1097-0...<1386::AID-CNCR2820360430>3.0.CO;2-7.
15.
Mutalik S, Mutalik VS, Pai KM, Naikmasur VG, Phaik KS. Oral Leukoplakia – Is Biopsy at the Initial Appointment a Must? J Clin Diagn Res. 2014; 8(8): ZC04–ZC07. http://doi.org/10.7860/JC DR / 2 014 /8 717. 4 6 59.
16.
Ghosh S, Pal S, Ghatak S, Saha S, Biswas S, Srivastava P. A Clinicopathologic and Epidemiologic Study of Chronic White Lesions in the Oral Mucosa. Ear Nose Throat J. 2017; 96(8): E13-E17. https://doi.org/10.1177/014556....
17.
Aghbari SMH, Abushouk AI, Attia A, Elmaraezy A, Menshawy A, Ahmed MS, et al. Malignant transformation of oral lichen planus and oral lichenoid lesions: A meta-analysis of 20095 patient data. Oral Oncol. 2017; 68: 92–102. https://doi.org/10.1016/j.oral... y.2017.03.012.
18.
González-Moles MÁ, Ruiz-Ávila I, González-Ruiz L, Ayén Á, Gil-Montoya JA, Ramos-García P. Malignant transformation risk of oral lichen planus: A systematic review and comprehensive meta-analysis. Oral Oncol. 2019; 96: 121–130. https://doi.org/10.1016/j.oral... y.2019.07.012.
19.
Bánóczy J, Csiba A. Comparative study of the clinical picture and histopathologic structure of oral leukoplakia. Cancer. 1972; 29(5): 1230–4. https://doi.org/10.1002/1097– 0142(197205)29:5<1230::AID-CNCR2820290515>3.0.CO;2-3.
20.
Stiewe T, Haran TE. How mutations shape p53 interactions with the genome to promote tumorigenesis and drug resistance. Drug Resist Updat. 2018; 38: 27–43. https://doi.org/10.1016/j.drup....
21.
Nagler R, Bahar G, Shpitzer T, Feinmesser R. Concomitant analysis of salivary tumor markers – a new diagnostic tool for oral cancer. Clin JPCCRJournal of Pre-Clinical and Clinical ResearchCancer Res. 2006; 12(13): 3979–84. https://doi.org/10.1158/1078-0....
22.
Woo SB1, Lin D. Morsicatio mucosae oris – a chronic oral frictional keratosis, not a leukoplakia. J Oral Maxillofac Surg. 2009; 67(1): 140-6. https://doi.org/10.1016/j.joms....
23.
Chi AC, Lambert III PR, Pan Y, Li R, Vo D-T, Edwards E, et al. Is alveolar ridge keratosis a true leukoplakia?: A clinicopathologic comparison of 2,153 lesions. J Am Dent Assoc. 2007; 138(5): 641–51. https://doi.org/10.14219/jada.....
24.
Schulman JD, Beach MM, Rivera-Hidalgo F. The prevalence of oral mucosal lesions in U.S. adults: data from the Third National Health and Nutrition Examination Survey, 1988–1994. J Am Dent Assoc 2004; 135: 1279–1286. https://doi.org/10.14219/jada.....
25.
Lee KH, Polonowita AD. Oral white lesions: pitfalls of diagnosis. Med J Aust. 2009; 190(5): 274–7.
26.
Williams PM1, Poh CF, Hovan AJ, Ng S, Rosin MP. Evaluation of a suspicious oral mucosal lesion. J Can Dent Assoc. 2008; 74(3): 275–80.
27.
Brouns EREA, Baart JA, Bloemena E, Karagozoglu H, van der Waal I. The relevance of uniform reporting in oral leukoplakia: Definition, certainty factor and staging based on experience with 275 patients. Med Oral Patol Oral Cir Bucal. 2013; 18 (1): e19–26. http://dx.doi.org/doi: 10.4317/medora l.18756.
28.
Reibel J. Prognosis of oral pre-malignant lesions: significance of clinical, histopathological, and molecular biological characteristics. Crit Rev Oral Biol Med. 2003; 14(1): 47–62. https://doi.org/10.1177/154411....
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.