Online first
About the Journal
Current issue
Archive
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Office
Editorial Board
Contact
Reviewers
All Reviewers
2024
2023
2022
2021
2020
2019
2018
2017
2016
2025
General Data Protection Regulation (RODO)
RESEARCH PAPER
Methods of unproved or uncertain effectiveness used by patients with Atopic Dermatitis
1
Dermatological Students Scientific Association, Department of Dermatology, Venereology and Allergology, Faculty of
Medicine, Medical University, Gdańsk, Poland
2
Faculty of Medicine, Medical University, Gdańsk, Poland
3
Department of Dermatology, Venereology and Allergology, Faculty of Medicine, Medical University, Gdańsk, Poland
Corresponding author
Alicja Mesjasz
Dermatological Students Scientific Association, Department of Dermatology, Venereology and Allergology, Faculty of Medicine, Medical University, 80–214, Gdansk, Poland
Dermatological Students Scientific Association, Department of Dermatology, Venereology and Allergology, Faculty of Medicine, Medical University, 80–214, Gdansk, Poland
J Pre Clin Clin Res. 2023;17(2):52-55
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Atopic dermatitis (AD) is a common, chronic, recurrent dermatosis. It frequently decreases the quality of life and leads to frustration of both patients and their families. Patients with AD seek a variety of therapeutic options, including non-conventional methods. The aim of the study was to determine which practices of unproved or uncertain effectiveness are most frequently used by AD patients in Poland.
Material and methods:
113 survey participants were enrolled (99 parents of children and 14 adults) in Poland diagnosed with AD who responded to an online survey created using Google Forms distributed to online support groups for parents of patients and patients diagnosed with AD. Respondents were given a list of methods of unproved or uncertain treatments for AD, and were asked to choose the methods that they had employed at least once in their lives to manage their or their children’s AD.
Results:
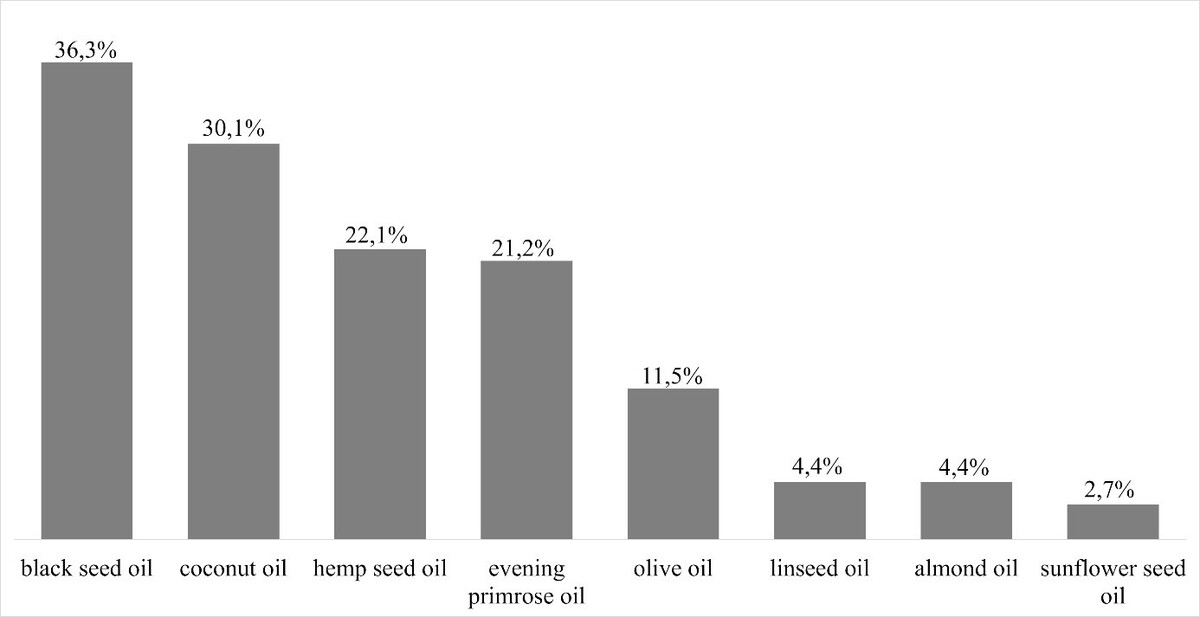
At least one method described in the study to manage AD had been tried by 76.1% of respondents. Black seed oil was the most popular pure oil, with up to 36.3% of respondents having tried it, making it as popular as cannabinoidcontaining ointments and creams. The use of propolis was reported by 24.8% of respondents. Acupuncture had been tried at least once by 23.9% of patients or parents of patients, while 18% attempted bioresonance.
Conclusions:
This study reveals that AD patients engage in a wide range of practices that contradict current knowledge and recommendations. Dissemination of reliable sources of information and insightful conversations in doctors’ offices about methods seem important.
Atopic dermatitis (AD) is a common, chronic, recurrent dermatosis. It frequently decreases the quality of life and leads to frustration of both patients and their families. Patients with AD seek a variety of therapeutic options, including non-conventional methods. The aim of the study was to determine which practices of unproved or uncertain effectiveness are most frequently used by AD patients in Poland.
Material and methods:
113 survey participants were enrolled (99 parents of children and 14 adults) in Poland diagnosed with AD who responded to an online survey created using Google Forms distributed to online support groups for parents of patients and patients diagnosed with AD. Respondents were given a list of methods of unproved or uncertain treatments for AD, and were asked to choose the methods that they had employed at least once in their lives to manage their or their children’s AD.
Results:
At least one method described in the study to manage AD had been tried by 76.1% of respondents. Black seed oil was the most popular pure oil, with up to 36.3% of respondents having tried it, making it as popular as cannabinoidcontaining ointments and creams. The use of propolis was reported by 24.8% of respondents. Acupuncture had been tried at least once by 23.9% of patients or parents of patients, while 18% attempted bioresonance.
Conclusions:
This study reveals that AD patients engage in a wide range of practices that contradict current knowledge and recommendations. Dissemination of reliable sources of information and insightful conversations in doctors’ offices about methods seem important.
FUNDING
Mesjasz A, Siemiątkowski P, Trzeciak M. Methods of unproved or uncertain effectiveness used by patients with Atopic Dermatitis. J Pre-Clin
Clin Res. 2023; 17(2): 52–55. doi: 10.26444/jpccr/163375
REFERENCES (37)
1.
Sroka-Tomaszewska J, Trzeciak M. Molecular mechanisms of atopic dermatitis pathogenesis. Int J Mol Sci. 2021;22(8). doi:10.3390/ijms22084130.
2.
Son JH, Chung BY, Kim HO, Park CW. Clinical Features of Atopic Dermatitis in Adults Are Different according to Onset. J Korean Med Sci. 2017;32(8):1360. doi:10.3346/JKMS.2017.32.8.1360.
3.
Kowalska-Olędzka E, Czarnecka M, Baran A. Epidemiology of atopic dermatitis in Europe. J Drug Assess. 2019;8(1):126. doi:10.1080/21556660.2019.1619570.
4.
Nutten S. Atopic Dermatitis: Global Epidemiology and Risk Factors. Ann Nutr Metab. 2015;66(Suppl. 1):8–16. doi:10.1159/000370220.
5.
Croce EA, Rew L. Sociocultural Influences on Disparities in United States Children with Atopic Dermatitis: A Narrative Review of the Literature. Compr Child Adolesc Nurs. 2020;44(4):239–254. doi:10.1080/24694193.2020.1799113.
6.
Ng JPX, Liew HM, Ang SB. Use of emollients in atopic dermatitis. Journal of the European Academy of Dermatology and Venereology. 2015;29(5):854–857. doi:10.1111/jdv.12864.
7.
Johnson BB, Franco AI, Beck LA, Prezzano JC. Treatment-resistant atopic dermatitis: challenges and solutions. Clin Cosmet Investig Dermatol. 2019;12:181. doi:10.2147/CCID.S163814.
8.
Lee JY, Her Y, Kim CW, Kim SS. Topical Corticosteroid Phobia among Parents of Children with Atopic Eczema in Korea. Ann Dermatol. 2015;27(5):499–506. doi:10.5021/AD.2015.27.5.499.
9.
Qiu J, Grine K. Complementary and Alternative Treatment for Allergic Conditions. Primary Care: Clinics in Office Practice. 2016;43(3):519–526. doi:10.1016/J.POP.2016.04.012.
10.
Niggemann B, Grüber C. Side-effects of complementary and alternative medicine. Allergy. 2003;58(8):707–716. doi:10.1034/J.1398–9995.2003.00219.X.
11.
Schäfer T. Complementary and alternative medicine (CAM) and atopic eczema. Allergol Select. 2017;1(1):44. doi:10.5414/ALX01287E.
12.
Holm JG, Clausen ML, Agner T, Thomsen SF. Use of Complementary and Alternative Therapies in Outpatients with Atopic Dermatitis from a Dermatological University Department. Dermatology. 2019;235(3):189–195. doi:10.1159/000496274.
13.
Johnston GA, Bilbao RM, Graham-Brown RAC. The use of complementary medicine in children with atopic dermatitis in secondary care in Leicester. British Journal of Dermatology. 2003;149(3):566–571. doi:10.1046/J.1365–2133.2003.05471.X.
14.
Koo K, Nagayah R, Begum S, Tuan Mahmood TM, Mohamed Shah N. The use of complementary and alternative medicine in children with atopic eczema at a tertiary care centre in Malaysia. Complement Ther Med. 2020;49:102355. doi:10.1016/J.CTIM.2020.102355.
15.
Khan S, Zagona-Prizio C, Yee D, et al. Complementary and alternative medicine use among adults with eczema: A population-based study. JAAD Int. 2022;8:154–156. doi:10.1016/J.JDIN.2022.05.013.
16.
Akbaş A, Emeksiz ZŞ, Yorulmaz A, et al. Complementary and alternative treatment methods practiced by parents in pediatric cases diagnosed with atopic dermatitis. https://doi.org/101080/0954663.... Published online 2022. doi:10.1080/09546634.2022.2097159.
17.
Wollenberg A, Kinberger M, Arents B, et al. European guideline (EuroGuiDerm) on atopic eczema – part II: non-systemic treatments and treatment recommendations for special AE patient populations. Journal of the European Academy of Dermatology and Venereology. Published online September 3, 2022. doi:10.1111/JDV.18429.
18.
Widyaswari MS, Noventi I, Supriyana H. Anti-eczema Mechanism of Action of Nigella sativa for Atopic Dermatitis: Computer-aided Prediction and Pathway Analysis Based on Protein-chemical Interaction Networks. Biomolecular and Health Science Journal. 2019;2(2):68. doi:10.20473/BHSJ.V2I2.15007.
19.
Karagounis TK, Gittler JK, Rotemberg V, Morel KD. Use of “natural” oils for moisturization: Review of olive, coconut, and sunflower seed oil. Pediatr Dermatol. 2019;36(1):9–15. doi:10.1111/PDE.13621.
20.
Sivesind TE, Maghfour J, Rietcheck H, Kamel K, Malik AS, Dellavalle RP. Cannabinoids for the Treatment of Dermatologic Conditions. JID Innov. 2022;2(2):100095. doi:10.1016/J.XJIDI.2022.100095.
21.
Vieira BL, Lim NR, Lohman ME, Lio PA. Complementary and Alternative Medicine for Atopic Dermatitis: An Evidence-Based Review. Am J Clin Dermatol. 2016;17(6):557–581. doi:10.1007/S40257–016–0209–1/TABLES/9.
22.
Wollenberg A, Barbarot S, Bieber T, et al. Consensus-based European guidelines for treatment of atopic eczema (atopic dermatitis) in adults and children: part II. Journal of the European Academy of Dermatology and Venereology. 2018;32(6):850–878. doi:10.1111/JDV.14888.
23.
Liew KY, Kamise NI, Ong HM, et al. Anti-Allergic Properties of Propolis: Evidence From Preclinical and Clinical Studies. Front Pharmacol. 2022;12. doi:10.3389/FPHAR.2021.785371/FULL.
24.
Alangari AA, Morris K, Lwaleed BA, et al. Honey is potentially effective in the treatment of atopic dermatitis: Clinical and mechanistic studies. Immun Inflamm Dis. 2017;5(2):190. doi:10.1002/IID3.153.
25.
Gaudin O, Toukal F, Hua C, et al. Association Between Severe Acute Contact Dermatitis Due to Nigella sativa Oil and Epidermal Apoptosis. JAMA Dermatol. 2018;154(9):1062. doi:10.1001/JAMADERMATOL.2018.2120.
26.
Yousefi M, Barikbin B, Kamalinejad M, et al. Comparison of therapeutic effect of topical Nigella with Betamethasone and Eucerin in hand eczema. J Eur Acad Dermatol Venereol. 2013;27(12):1498–1504. doi:10.1111/JDV.12033.
27.
Tan HY, Lenon GB, Zhang AL, Xue CC. Efficacy of acupuncture in the management of atopic dermatitis: a systematic review. Clin Exp Dermatol. 2015;40(7):711–716. doi:10.1111/CED.12732.
28.
Schöni MH, Nikolaizik WH, Schöni-Affolter F. Efficacy trial of bioresonance in children with atopic dermatitis. Int Arch Allergy Immunol. 1997;112(3):238–246. doi:10.1159/000237460.
29.
Schäfer T. Complementary and alternative medicine (CAM) and atopic eczema. Allergol Select. 2017;1(1):45. doi:10.5414/ALX01287E.
30.
Al-Waili NS. Topical application of natural honey, beeswax and olive oil mixture for atopic dermatitis or psoriasis: partially controlled, single-blinded study. Complement Ther Med. 2003;11(4):226–234. doi:10.1016/S0965–2299(03)00120–1.
31.
Gu S, Yang AWH, Xue CCL, et al. Chinese herbal medicine for atopic eczema. Cochrane Database Syst Rev. 2013;2013(9). doi:10.1002/14651858.CD008642.PUB2.
32.
Chan K, Zhang H, Lin ZX. An overview on adverse drug reactions to traditional Chinese medicines. Br J Clin Pharmacol. 2015;80(4):834. doi:10.1111/BCP.12598.
33.
Smith SD, Hong E, Fearns S, Blaszczynski A, Fischer G. Corticosteroid phobia and other confounders in the treatment of childhood atopic dermatitis explored using parent focus groups. Australasian Journal of Dermatology. 2010;51(3):168–174. doi:10.1111/j.1440–0960.2010.00636.x.
34.
Avila C, Massick S, Kaffenberger BH, Kwatra SG, Bechtel M. Cannabinoids for the treatment of chronic pruritus: A review. J Am Acad Dermatol. 2020;82(5):1205–1212. doi:10.1016/J.JAAD.2020.01.036.
35.
Kim JE, Kim HJ, Lew BL, et al. Consensus Guidelines for the Treatment of Atopic Dermatitis in Korea (Part I): General Management and Topical Treatment. Ann Dermatol. 2015;27(5):563–577. doi:10.5021/AD.2015.27.5.563.
36.
Bath-Hextall FJ, Jenkinson C, Humphreys R, Williams HC. Dietary supplements for established atopic eczema. Cochrane Database Syst Rev. 2012;2012(2). doi:10.1002/14651858.CD005205.PUB3.
37.
Jonas WB, Kaptchuk TJ, Linde K. A critical overview of homeopathy. Ann Intern Med. 2003;138(5):393–399. doi:10.7326/0003–4819–138–5–200303040–00009.
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.