CASE REPORT
Importance of early intervention in verapamil overdose – Case Report and antidotes review
1
Department of Pathophysiology, Medical University of Lublin, Poland
2
Student’s Research Group at the Department of Toxicology, Medical University of Lublin, Poland
3
Department of Toxicology, Medical University of Lublin, Poland
Corresponding author
Małgorzata Drozd
Student’s Research Group at the Department of Toxicology, Medical University of Lublin, Lublin, Poland
Student’s Research Group at the Department of Toxicology, Medical University of Lublin, Lublin, Poland
J Pre Clin Clin Res. 2021;15(3):142-147
KEYWORDS
overdosecalcium channel blockerhigh-dose insulinverapamil intoxicationtoxicologylipid emulsion therapyantidotes
TOPICS
ABSTRACT
Introduction:
Verapamil is a widely used cardiac drug. It belongs to the non-dihydropiridine subgroup of calcium channel blockers (CCBs), and is used mainly for the treatment of atrial dysrhythmias, hypertension or angina. In this article, we describe a case of poisoning with verapamil mixed with ethanol and review current treatment options. A 54-year-old female was admitted to the Toxicology Clinic by emergency medical services after ingesting sustained-release CCBs and ethanol in a suicidal attempt. The patient was successfully treated by administration of catecholamines and calcium, and the introduction of a high-dose insulin infusion (HDI).
Conclusions:
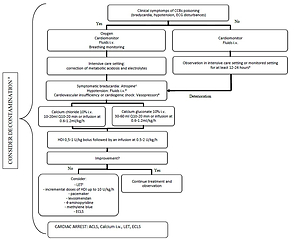
This case report emphasizes that even in severe poisoning, early and proper intervention may prevent circulatory breakdown. It also summarizes treatment options in patients after verapamil overdose. Along with decontamination, administration of catecholamines and correcting electrolyte abnormalities, the main options are HDI and lipid emulsion therapy (LET)
Verapamil is a widely used cardiac drug. It belongs to the non-dihydropiridine subgroup of calcium channel blockers (CCBs), and is used mainly for the treatment of atrial dysrhythmias, hypertension or angina. In this article, we describe a case of poisoning with verapamil mixed with ethanol and review current treatment options. A 54-year-old female was admitted to the Toxicology Clinic by emergency medical services after ingesting sustained-release CCBs and ethanol in a suicidal attempt. The patient was successfully treated by administration of catecholamines and calcium, and the introduction of a high-dose insulin infusion (HDI).
Conclusions:
This case report emphasizes that even in severe poisoning, early and proper intervention may prevent circulatory breakdown. It also summarizes treatment options in patients after verapamil overdose. Along with decontamination, administration of catecholamines and correcting electrolyte abnormalities, the main options are HDI and lipid emulsion therapy (LET)
FUNDING
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. The authors have no disclosures to declare.
Marzęda P, Drozd M, Tchórz M, Kisiel K. Importance of early intervention in verapamil overdose. Case report and antidotes review. J Pre-Clin
Clin Res. 2021; 15(3): 142–147. doi: 10.26444/jpccr/139037
REFERENCES (64)
1.
Godfraind T. Discovery and Development of Calcium Channel Blockers. Front Pharmacol. 2017; 8: 286. doi: 10.3389/fphar.2017.00286.
2.
Rirash F, Tingey PC, Harding SE, et al. Calcium channel blockers for primary and secondary Raynaud’s phenomenon. Cochrane Database Syst Rev. 2017; 12: CD000467. doi: 10.1002/14651858.CD000467.pub2.
3.
Chakraborty RK, Hamilton RJ. Calcium Channel Blocker Toxicity. StatPearls Publishing; 2018.
4.
Striessnig J, Ortner N, Pinggera A. Pharmacology of L-type Calcium Channels: Novel Drugs for Old Targets? Curr Mol Pharmacol. 2015; 8(2): 110–122. doi: 10.2174/1874467208666150507105845.
5.
Rorsman P, Ashcroft FM. Pancreatic β-Cell Electrical Activity and Insulin Secretion: Of Mice and Men. Physiol Rev. 2018; 98(1): 117–214. doi: 10.1152/physrev.00008.2017.
6.
Rizos C V, Elisaf MS. Antihypertensive drugs and glucose metabolism. World J Cardiol. 2014; 6(7): 517–530. doi: 10.4330/wjc.v6.i7.517.
7.
Noto H, Goto A, Tsujimoto T, Noda M. Effect of calcium channel blockers on incidence of diabetes: a meta-analysis. Diabetes Metab Syndr Obes Targets Ther. 2013; 6: 257–261. doi: 10.2147/DMSO.S49767.
8.
Gummin DD, Mowry JB, Beuhler MC, et al. 2019 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 37th Annual Report. Clin Toxicol. 2020; 58(12): 1360–1541. doi: 10.1080/15563650.2020.1834219.
9.
Christensen MB, Petersen KM, Bøgevig S, et al. Outcomes following calcium channel blocker exposures reported to a poison information center. BMC Pharmacol Toxicol. 2018; 19. doi: 10.1186/s40360-018-0271-9.
10.
Mandigers L, Bollen PDJ, Bijlstra PJ, Brands E. Severe verapamil intoxication despite correct use of low-dose verapamil. Drug Metab Pers Ther. 2016; 31(1): 55–58. doi: 10.1515/dmpt-2015-0041.
12.
Bartlett JW, Walker PL. Management of Calcium Channel Blocker Toxicity in the Pediatric Patient. J Pediatr Pharmacol Ther JPPT. 2019; 24(5): 378–389. doi: 10.5863/1551-6776-24.5.378.
13.
Kline JA, Raymond RM, Schroeder JD, Watts JA. The Diabetogenic Effects of Acute Verapamil Poisoning. Toxicol Appl Pharmacol. 1997; 145(2): 357–362. doi: 10.1006/taap.1997.8195.
14.
Levine M, Boyer EW, Pozner CN, et al. Assessment of hyperglycemia after calcium channel blocker overdoses involving diltiazem or verapamil. Crit Care Med. 2007; 35(9): 2071–2075. doi: 10.1097/01.ccm.0000278916.04569.23.
15.
Siddiqi TA, Hill J, Huckleberry Y, Parthasarathy S. Non-cardiogenic pulmonary edema and life-threatening shock due to calcium channel blocker overdose: a case report and clinical review. Respir Care. 2014; 59(2): e15–21. doi: 10.4187/respcare.02244.
16.
Izdes S, Altintas ND, Soykut C. Acute respiratory distress syndrome after verapamil intoxication: case report and literature review. Acta Clin Belg. 2014; 69(2): 116–119. doi: 10.1179/2295333714Y.0000000007.
17.
Lodhi FAK, Shogren SL, Vedre JG, Haque N, Reriani M, Ali R. Calcium Channel Blocker Toxicity Causing Acute Respiratory Distress Syndrome: A Commonly Used Drug Triggering a Life-Threatening Condition. WMJ Off Publ State Med Soc Wis. 2020; 119(1): 66–68.
18.
Charpentier C, Flandrois M, Labombarda F, Maragnes P, Jokic M, Villedieu F. Intoxication aigüe au vérapamil: attention à l’effet retard. Arch Pédiatrie. 2014; 21(12): 1344–1347. doi: 10.1016/j.arcped.2014.09.013.
19.
Tuka V, Ricarova B, Janota T, Malik J, Kotrlikova E. Surprisingly delayed escalation of severe verapamil poisoning. Eur J Emerg Med. 2009; 16(2): 100–102. doi: 10.1097/MEJ.0b013e32830a997c.
20.
Chan L-N, Anderson GD. Pharmacokinetic and pharmacodynamic drug interactions with ethanol (alcohol). Clin Pharmacokinet. 2014; 53(12): 1115–1136. doi: 10.1007/s40262-014-0190-x.
21.
St-Onge M, Anseeuw K, Cantrell FL, et al. Experts Consensus Recommendations for the Management of Calcium Channel Blocker Poisoning in Adults. Crit Care Med. 2017; 45(3): e306-e315. doi: 10.1097/CCM.0000000000002087.
22.
Mégarbane B, Oberlin M, Alvarez J-C, et al. Management of pharmaceutical and recreational drug poisoning. Ann Intensive Care. 2020; 10(1): 157. doi: 10.1186/s13613-020-00762-9.
23.
Rietjens SJ, de Lange DW, Donker DW, Meulenbelt J. Practical recommendations for calcium channel antagonist poisoning. Neth J Med. 2016; 74(2): 8.
24.
Truhlář A, Deakin CD, Soar J, et al. European Resuscitation Council Guidelines for Resuscitation 2015. Resuscitation. 2015; 95: 148–201. doi: 10.1016/j.resuscitation.2015.07.017.
25.
Thanacoody R, Caravati EM, Troutman B, et al. Position paper update: Whole bowel irrigation for gastrointestinal decontamination of overdose patients. Clin Toxicol. 2015; 53(1): 5–12. doi: 10.3109/15563650.2014.989326.
26.
Lashari BH, Minalyan A, Khan W, Naglak M, Ward W. The Use of High-dose Insulin Infusion and Lipid Emulsion Therapy in Concurrent Beta-blocker and Calcium Channel Blocker Overdose. Cureus. 2018; 10(11): e3534. doi: 10.7759/cureus.3534.
27.
Dubé L, Granry JC. The therapeutic use of magnesium in anesthesiology, intensive care and emergency medicine: a review. Can J Anaesth. 2003 Aug-Sep; 50(7): 732–46. doi: 10.1007/BF03018719. PMID: 12944451.
28.
Woodward C, Pourmand A, Mazer-Amirshahi M. High dose insulin therapy, an evidence based approach to beta blocker/calcium channel blocker toxicity. Daru J Fac Pharm Tehran Univ Med Sci. 2014; 22(1): 36. doi: 10.1186/2008-2231-22-36.
29.
Krenz JR, Kaakeh Y. An Overview of Hyperinsulinemic-Euglycemic Therapy in Calcium Channel Blocker and β-blocker Overdose. Pharmacother J Hum Pharmacol Drug Ther. 2018; 38(11): 1130–1142. doi: 10.1002/phar.2177.
30.
Cole JB, Arens AM, Laes JR, Klein LR, Bangh SA, Olives TD. High dose insulin for beta-blocker and calcium channel-blocker poisoning. Am J Emerg Med. 2018; 36(10): 1817–1824. doi: 10.1016/j.ajem.2018.02.004.
31.
Walter E, McKinlay J, Corbett J, Kirk-Bayley J. Review of management in cardiotoxic overdose and efficacy of delayed intralipid use. J Intensive Care Soc. 2018; 19(1): 50–55. doi: 10.1177/1751143717705802.
32.
Cole JB, Stellpflug SJ, Ellsworth H, et al. A blinded, randomized, controlled trial of three doses of high-dose insulin in poison-induced cardiogenic shock. Clin Toxicol. 2013; 51(4): 201–207. doi: 10.3109/15563650.2013.770152.
33.
Holger JS, Stellpflug SJ, Cole JB, Harris CR, Engebretsen KM. High-dose insulin: A consecutive case series in toxin-induced cardiogenic shock. Clin Toxicol. 2011; 49(7): 653–658. doi: 10.3109/15563650.2011.593522.
34.
Wong A, Hoffman RS, Walsh SJ, et al. Extracorporeal treatment for calcium channel blocker poisoning: systematic review and recommendations from the EXTRIP workgroup. Clin Toxicol. 2021; 0(0): 1–31. doi: 10.1080/15563650.2020.1870123.
35.
Lashari BH, Minalyan A, Khan W, Naglak M, Ward W. The Use of High-dose Insulin Infusion and Lipid Emulsion Therapy in Concurrent Beta-blocker and Calcium Channel Blocker Overdose. Cureus. 2018; 10(11): e3535. doi: 10.7759/cureus.3534.
36.
Ciechanowicz S, Patil V. Lipid emulsion for local anesthetic systemic toxicity. Anesthesiol Res Pract. 2012; 2012: 131784. doi: 10.1155/2012/131784.
37.
Sampson CS, Bedy S-M. Lipid emulsion therapy given intraosseously in massive verapamil overdose. Am J Emerg Med. 2015; 33(12): 1844.e1. doi: 10.1016/j.ajem.2015.04.061.
38.
Doepker B, Healy W, Cortez E, Adkins EJ. High-Dose Insulin and Intravenous Lipid Emulsion Therapy for Cardiogenic Shock Induced by Intentional Calcium-Channel Blocker and Beta-Blocker Overdose: A Case Series. J Emerg Med. 2014; 46(4): 486–490. doi: 10.1016/j.jemermed.2013.08.135.
39.
Young AC, Velez LI, Kleinschmidt KC. Intravenous fat emulsion therapy for intentional sustained-release verapamil overdose. Resuscitation. 2009; 80(5): 591–593. doi: 10.1016/j.resuscitation.2009.01.023.
40.
French D, Armenian P, Ruan W, et al. Serum verapamil concentrations before and after Intralipid® therapy during treatment of an overdose. Clin Toxicol. 2011; 49(4): 340–344. doi: 10.3109/15563650.2011.572556.
41.
Kang C, Kim DH, Kim SC, et al. The effects of intravenous lipid emulsion on prolongation of survival in a rat model of calcium channel blocker toxicity. Clin Toxicol. 2015; 53(6): 540–544. doi: 10.3109/15563650.2015.1045979.
42.
Sebe A, Dişel NR, Açıkalın Akpınar A, Karakoç E. Role of intravenous lipid emulsions in the management of calcium channel blocker and β-blocker overdose: 3 years experience of a university hospital. Postgrad Med. 2015; 127(2): 119–124. doi: 10.1080/00325481.2015.1012480.
43.
Levine M, Hoffman RS, Lavergne V, et al. Systematic review of the effect of intravenous lipid emulsion therapy for non-local anesthetics toxicity. Clin Toxicol. 2016; 54(3): 194–221. doi: 10.3109/15563650.2015.1126286.
44.
Cao D, Heard K, Foran M, Koyfman A. Intravenous lipid emulsion in the emergency department: a systematic review of recent literature. J Emerg Med. 2015; 48(3): 387–397. doi: 10.1016/j.jemermed.2014.10.009.
45.
Pathak A, Lebrin M, Vaccaro A, Senard JM, Despas F. Pharmacology of levosimendan: inotropic, vasodilatory and cardioprotective effects. J Clin Pharm Ther. 2013; 38(5): 341–349. doi: 10.1111/jcpt.12067.
46.
Abraham MK, Scott SB, Meltzer A, Barrueto F. Levosimendan does not improve survival time in a rat model of verapamil toxicity. J Med Toxicol Off J Am Coll Med Toxicol. 2009; 5(1): 3–7.
47.
Osthoff M, Bernsmeier C, Marsch SC, Hunziker PR. Levosimendan as treatment option in severe verapamil intoxication: a case report and review of the literature. Case Rep Med. 2010; 2010. doi: 10.1155/2010/546904.
48.
Glinka L, Mayzner-Zawadzka E, Onichimowski D, Jalali R, Glinka M. Levosimendan in the modern treatment of patients with acute heart failure of various aetiologies. Arch Med Sci AMS. 2019; 17(2): 296–303. doi: 10.5114/aoms.2018.77055.
49.
St-Onge M, Dubé P-A, Gosselin S, et al. Treatment for calcium channel blocker poisoning: a systematic review. Clin Toxicol Phila Pa. 2014; 52(9): 926 –944. doi: 10.3109/15563650.2014.965827.
50.
Bellou A, Al-Hammadi S, Aburawi EH, et al. 4-Aminopyridine, A Blocker of Voltage-Dependent K+ Channels, Restores Blood Pressure and Improves Survival in the Wistar Rat Model of Anaphylactic Shock. Crit Care Med. 2016; 44(11): e1082-e1089. doi: 10.1097/CCM.0000000000001822.
51.
Fiszer M, Kołaciński Z, Rechciński T. [The application of 4-aminopyridine in calcium channel inhibitors acute poisoning]. Przegl Lek. 2007; 64(4–5): 293–297.
52.
Magdalan J, Kochman K, Antończyk A, Przewłocki M, Smolarek M. [Successful treatment by 4--aminopyridine of three cases of severe verapamil poisoning]. Przegl Lek. 2003; 60(4): 271–273.
53.
Warrick BJ, Tataru AP, Smolinske S. A systematic analysis of methylene blue for drug-induced shock. Clin Toxicol. 2016; 54(7): 547–555. doi: 10.1080/15563650.2016.1180390.
54.
Jang DH, Nelson LS, Hoffman RS. Methylene Blue for Distributive Shock: A Potential New Use of an Old Antidote. J Med Toxicol. 2013; 9(3): 242–249. doi: 10.1007/s13181-013-0298-7.
55.
Jang DH, Donovan S, Nelson LS, Bania TC, Hoffman RS, Chu J. Efficacy of Methylene Blue in an Experimental Model of Calcium Channel Blocker–Induced Shock. Ann Emerg Med. 2015; 65(4): 410–415. doi: 10.1016/j.annemergmed.2014.09.015.
56.
Ahmed S, Barnes S. Hemodynamic improvement using methylene blue after calcium channel blocker overdose. World J Emerg Med. 2019; 10(1): 55–58. doi: 10.5847/wjem.j.1920-8642.2019.01.009.
57.
Laes JR, Williams DM, Cole JB. Improvement in Hemodynamics After Methylene Blue Administration in Drug-Induced Vasodilatory Shock: A Case Report. J Med Toxicol. 2015; 11(4): 460–463. doi: 10.1007/s13181-015-0500-1.
58.
Saha BK, Bonnier A, Chong W. Rapid reversal of vasoplegia with methylene blue in calcium channel blocker poisoning. Afr J Emerg Med Rev Afr Med Urgence. 2020; 10(4): 284–287. doi: 10.1016/j.afjem.2020.06.014.
59.
Ginimuge PR, Jyothi SD. Methylene blue: revisited. J Anaesthesiol Clin Pharmacol. 2010; 26(4): 517–520.
60.
Groot M, Grewal S, Meeder H, Thiel R, den Uil C. Extracorporeal life support in calcium antagonist intoxication. Ned Tijdschr Geneeskd. 2017; 161: D1960.
61.
de Lange DW, Sikma MA, Meulenbelt J. Extracorporeal membrane oxygenation in the treatment of poisoned patients. Clin Toxicol Phila Pa. 2013; 51(5): 385–393. doi: 10.3109/15563650.2013.800876.
62.
Mégarbane B, Karyo S, Abidi K, et al. Predictors of Mortality in Verapamil Overdose: Usefulness of Serum Verapamil Concentrations. Basic Clin Pharmacol Toxicol. 2011; 108(6): 385–389. doi: 10.1111/j.1742-7843.2010.00666.x.
63.
Morini L, Moretti M, Brandolini F, Osculati AMM, Groppi A, Vignali C. Two Fatal Cases Involving Cardiovascular Drugs Diltiazem and Amlodipine. J Anal Toxicol. 2018; 42(1): e15-e19. doi: 10.1093/jat/bkx087.
64.
Szpak D. Zatrucia lekami i innymi ksenobiotykami działającymi na układ krążenia. In: Jurowski K, Piekoszewski, editors. Toksykologia. Ed. 1. Warszawa; 2020. p. 418–424.
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.