CASE REPORT
Gingival enlargement induced by anticonvulsant drugs in children with microcephaly – Case Report
1
State University of Southwest Bahia, Jequié, Brazil
Corresponding author
Maislla Mayara Silva Ramos
State University of Southwest Bahia, Av. José Moreira Sobrinho, 45205-490, Jequié, Brazil
State University of Southwest Bahia, Av. José Moreira Sobrinho, 45205-490, Jequié, Brazil
J Pre Clin Clin Res. 2024;18(2):135-138
KEYWORDS
TOPICS
ABSTRACT
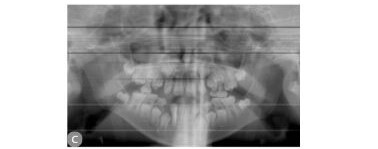
Microcephaly, in addition to craniofacial disproportion, can lead to skeletal muscle dysfunctions in the foetus, hearing and
visual alterations, as well as seizures and epilepsy. It is additionally important to note that the oral health of these children
can be compromised due to the difficulty in controlling mouth movements and chewing. Children have been taking
anticonvulsant drugs to control seizures and epilepsy since the first year of life. But will children with microcephaly who take
these drugs long term have oral manifestations from these substances? Could the delay in dental development be related
to a possible excess of gingival growth, preventing tooth eruption? Based on these questions, five clinical cases of children
with severe microcephaly, aged between seven and eight years in the mixed dentition stage, are presented, focusing on
gingival health and dental development.
Maislla Mayara Silva Ramos, Anna Liz Oliveira, Maria Letícia Velame, Adriano Monteiro d’Almeida Monteiro, Rita de Cássia Andrade, Maria da
Conceição Freitas. Gingival enlargement induced by anticonvulsant drugs in children with microcephaly: case reports. J Pre-Clin Clin Res.
2024; 18(2): 135–138. Doi: 10.26444/jpccr/187945
REFERENCES (18)
1.
Carvalho G, Ximenes A, Montarroyos R, et al. Early epilepsy in children with Zika-related microcephaly in a cohort in Recife, Brazil: Characteristics, electroencephalographic findings, and treatment response. Epilepsia. 61(3):509–18. https://pubmed.ncbi.nlm.nih. gov/32065676/ (access: 2020.03.01).
2.
Brasil. Nota Informativa N0 01/2015 – COES MICROCEFALIAS EMERGÊNCIA DE SAÚDE PÚBLICA DE IMPORTANCIA NACIONAL -ESPIN. https://saude.campinas.sp.gov.... Nota_MICROCEFALIAS_17_nov_2015.pdf (access: 2023.10.14).
3.
Gallo C, Bonvento G, Zagotto G, et al. Gingival overgrowth induced by anticonvulsant drugs: A cross-sectional study on epileptic patients. J Periodontal Res. 2021 Apr; 56(2):363–369. doi:10.1111/jre.12828. Epub 2020 Dec 23. PMID: 33368283 (access: 2023.10.14).
4.
Brown R, Arany P. Mechanism of drug-induced gingival overgrowth revisited: a unifying hypothesis. Oral Diseases. 2014 Aug 7;21(1):e51–61. doi:10.1111/odi.12264.
5.
Tungare S, Paranjpe G. Drug Induced Gingival Overgrowth (DIGO) [Internet]. PubMed. Treasure Island (FL): StatPearls Publishing; 2020. https://www.ncbi.nlm.nih.gov/b... (access: 2023.10.14).
6.
Caton G, Armitage G, Berglundh T, et al. A new classification scheme for periodontal and peri-implant diseases and conditions – Introduction and key changes from the 1999 classification. Journal of Clinical Periodontology. 2018 Jun;45:S1–8. https://onlinelibrary.wiley.co... full/10.1111/jcpe.12935 (access: 2023.10.14).
7.
Gusmão L, Faria S de, Leão C, et al. Dental changes in children with congenital Zika syndrome. Oral Diseases. 2020 Mar 1;26(2):457–64. Available from: https://pubmed.ncbi.nlm.nih.go... (access: 2023.07.13).
8.
Gomes N, Amaral A, Azevedo D, et al. Association of congenital Zika syndrome with dental alterations in children with microcephaly. PLOS ONE. 2022 Nov 1;17(11): e0276931–1. https://journals.plos.org/plos... article?id=10.1371/journal.pone.0276931 (access: 2023.07.13).
9.
Cavalcanti A. Challenges of dental care for children with microcephaly carrying Zika congenital syndrome. Contemporary Clinical Dentistry. 2017;8(3):345. https://www.ncbi.nlm.nih.gov/p... PMC5643986/ (access: 2023.07.13).
10.
Hatahira H, Abe J, Hane Y, et al. Drug-induced gingival hyperplasia: a retrospective study using spontaneous reporting system databases. Journal of Pharmaceutical Health Care and Sciences. 2017;3(3):19. https://pubmed.ncbi.nlm.nih.go... (access: 2023.10.14). 11. Zhang R, Wu J, Zhu J, et al. Bibliometric analysis of research trends and characteristics of drug-induced gingival overgrowth. Frontiers in Public Health. 2022 Sep 6;10. https://pubmed.ncbi.nlm.nih.go... (access: 2023.07.13).
11.
Murakami S, Mealey BL, Mariotti A, et al. Dental plaque-induced gingival conditions. Journal of Clinical Periodontology. 2018.
13.
Doufexi A, Mina M, Ioannidou E. Gingival Overgrowth in Children: Epidemiology, Pathogenesis, and Complications. A Literature Review. Journal of Periodontology. 2005 Jan;76(1):3–10. https://aap.onlinelibrary. wiley.com/doi/abs/10.1902/jop.2005.76.1.3 (access: 2023.10.14).
14.
Perucca P, Bahlo M, Berkovic SF. The Genetics of Epilepsy. Annual Review of Genomics and Human Genetics. 2020 Aug 31;21(1):205–30 https://pubmed.ncbi.nlm.nih.go... (access: 2023.10.14).
15.
Droździk A, Droździk M. Drug-Induced Gingival Overgrowth— Molecular Aspects of Drug Actions. International Journal of Molecular Sciences. 24(6):5448 https://www.mdpi.com/1422–0067...: 2023.10.14).
16.
Samudrala P, Chava V, Chandana T, et al. Drug-induced gingival overgrowth: A critical insight into case reports from over two decades. Journal of Indian Society of Periodontology. 2016;20(5):496. Available from: https://www.ncbi.nlm.nih.gov/p... (access: 2023.10.14).
17.
López GFJ, Rodríguez OX, Gil-NRA, et al. Epilepsia resistente a fármacos. Concepto y alternativas terapéuticas. Neurología. 2015 Sep;30(7):439–46. https://www.sciencedirect.com/... S0213485314001200 (access: 2023.10.14).
18.
Mawardi H, Alsubhi A, Salem N, et al. Management of medication- induced gingival hyperplasia: a systematic review. Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology. 2021 Jan;131(1):62–72. https://pubmed.ncbi.nlm.nih.go... (access: 2023.10.14).
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.