RESEARCH PAPER
Evaluation of the safety and effects of pregabalin premedication on sleep quality, haemodynamic changes and pain in elderly patients with comorbidities undergoing spinal stenosis
1
Training and Research Hospital, Umraniye, Turkey
J Pre Clin Clin Res. 2020;14(4):111-116
KEYWORDS
Elderlyspinal stenosispregabalinhaemodynamic changesintraoperative aaesthesia consumptionpostoperative analgesia
TOPICS
ABSTRACT
Objective:
The aim of the study was to determine the effects of pregabalin premedication on preoperative sleep quality, intraoperative haemodynamic parameters, anesthesia consumption, blood loss, and postoperative pain control in patients over 65 years of age who had undergone surgery for spinal stenosis. The study also aimed to determine whether pregabalin premedication was safe for that age group and compare its effects with those of diazepam.
Material and methods:
The retrospective study was conducted in a single centre after approval by the local Ethics Committee. The study sample consisted of 95 patients over 65 years of age who had undergone surgery for spinal stenosis. The sample was divided into two groups: Pregabalin premedication patients (PG; n = 45) and Diazepam patients (D; n = 51). Demographic data, American Society of Anesthesiologists (ASA) scores, comorbidities, indications for operation, pre-operative sleep quality, total anaesthesia consumption during surgery, intraoperative haemodynamic parameters and blood loss, time to leaving the post- anaesthetic care unit (Aldrete’s > 9), postoperative visual analog pain scale (VAS), total fentanyl consumption via a patient-controlled analgesia (PCA) device, additional demand for analgesic, first mobilization, first oral intake, and side-effects were recorded.
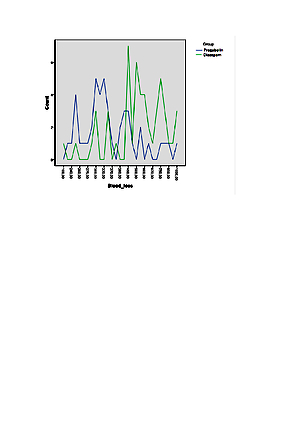
Results:
Participants did not significantly differ by demographic data and duration of surgery. The PG group had better sleep quality, lower systolic and diastolic blood pressure, heart rate, intraoperative bleeding, postoperative VAS scores, additional analgesic consumption, and total fentanyl consumption via a PCA, and earlier mobilization and oral intake than the D group. No serious side-effects were observed in the groups.
Conclusions:
Pregabalin premedication is a safe and effective alternative medication for patients over 65 years of age.
The aim of the study was to determine the effects of pregabalin premedication on preoperative sleep quality, intraoperative haemodynamic parameters, anesthesia consumption, blood loss, and postoperative pain control in patients over 65 years of age who had undergone surgery for spinal stenosis. The study also aimed to determine whether pregabalin premedication was safe for that age group and compare its effects with those of diazepam.
Material and methods:
The retrospective study was conducted in a single centre after approval by the local Ethics Committee. The study sample consisted of 95 patients over 65 years of age who had undergone surgery for spinal stenosis. The sample was divided into two groups: Pregabalin premedication patients (PG; n = 45) and Diazepam patients (D; n = 51). Demographic data, American Society of Anesthesiologists (ASA) scores, comorbidities, indications for operation, pre-operative sleep quality, total anaesthesia consumption during surgery, intraoperative haemodynamic parameters and blood loss, time to leaving the post- anaesthetic care unit (Aldrete’s > 9), postoperative visual analog pain scale (VAS), total fentanyl consumption via a patient-controlled analgesia (PCA) device, additional demand for analgesic, first mobilization, first oral intake, and side-effects were recorded.
Results:
Participants did not significantly differ by demographic data and duration of surgery. The PG group had better sleep quality, lower systolic and diastolic blood pressure, heart rate, intraoperative bleeding, postoperative VAS scores, additional analgesic consumption, and total fentanyl consumption via a PCA, and earlier mobilization and oral intake than the D group. No serious side-effects were observed in the groups.
Conclusions:
Pregabalin premedication is a safe and effective alternative medication for patients over 65 years of age.
FUNDING
No financial or support was received from any pharmaceutical company that had a direct connection with the research.
CONFLICT OF INTEREST
The authors declare that they have no conflicts of interest.
Ebru Tarıkçı Kılıç. Evaluation of the safety and the effects of pregabalin premedication on sleep quality, hemodynamic changes and pain in the elderly patients with comorbidities undergoing spinal stenosis. J Pre-Clin Clin Res. 2020; 14(4): 111–116. doi: 10.26444/jpccr/127924
REFERENCES (26)
1.
Ayşin Ersoy, Menşure Yılmaz Çakırgöz, Ülkü Aygen Türkmen. Geriatric Anesthesia. Okmeydanı Medical Journal. 2013; 29(2): 106–109.
2.
Kowark A, Rossaint R, Keszei AP, Bischoff P, Czaplik M, Drexler B, et al. Impact of Preoperative Midazolam on Outcome of Elderly patients (I-PROMOTE): study protocol for a multicentre randomised controlled trial. Trials. 2019 Jul 15; 20(1): 430.
3.
Wolfe JD1, Wolfe NK1, Rich MW1. Perioperative care of the geriatric patient for noncardiac surgery. Clin Cardiol. 2020 Feb; 43(2): 127–136. doi: 10.1002/clc.23302.
4.
Andres TM1, McGrane T2, McEvoy MD3, Allen BFS4. Geriatric Pharmacology: An Update. Anesthesiol Clin. 2019 Sep; 37(3): 475–492.
5.
Nabavighadi K, Batista C, Ghoddoussi F, Kumar N, Aiello A, Reeves B, Krishnan S, Ellis T 2nd. Oral multimodal preemptive analgesia improves postoperative pain control and decreases opioid utilization in spinal fusion patients. J Clin Anesth. 2020 May; 61: 109679.
6.
Woolf CJ, Chong MS. Preemptive analgesia – treating postoperative pain by preventing the establishment of central sensitization. Anesth Analg. 1993 Aug; 77(2): 362–79.
7.
Sills GJ, Rogawski MA. Mechanisms of action of currently used antiseizure drugs. Neuropharmacology. 2020 May 15; 168: 107966.
8.
Polat Bora S, Kol Özdemir İ, Avcı O, İşbir A, Kaygusuz K, Gürsoy S. Evaluation of Preoperative Anxiolytic and Postoperative Analgesic Effects of Pregabalin Premedication. Turkiye Klinikleri J Med Sci. 2019; 39(1): 9–18.
9.
Karube N, Ito S, Sako S, Hirokawa J, Yokoyama T. Sedative effects of oral pregabalin premedication on intravenous sedation using propofol target-controlled infusion. J Anesth. 2017 Aug; 31(4): 586–592.
10.
Christopher W, Goodman Allan S Brett. Gabapentin and Pregabalin for Pain – Is Increased Prescribing a Cause for Concern? N Engl J Med 2017; 377: 411–414.
11.
Gonano C, Latzke D, Sabeti-Aschraf M, Kettner SC, Chiari A, Gustorff B. The anxiolytic effect of pregabalin in outpatients undergoing minor orthopaedic surgery. J Psychopharmacol. 2011 Feb; 25(2): 249–51.
12.
Amany F Omara, Sameh A Ahmed, Motaz MA Abusabaa. The Effect Of The Use Of Pre-Emptive Oral Pregabalin On The Postoperative Spinal Analgesia In Patients Presented For Orthopedic Surgeries: Randomized Controlled Trial. J Pain Res. 2019; 12: 2807–2814.
13.
H Luo Z-Y Feng. A review of pregabalin in the treatment of post-operative pain. Chinese Journal of new drugs 22(8): 915–918.
14.
Dheer Singh, Jaybrijesh Singh Yadav, Birendra Kumar Jamuda, and Pooja Singh. Oral Pregabalin as Premedication on Anxiolysis and Stress Response to Laryngoscopy and Endotracheal Intubation in Patients Undergoing Laparoscopic Cholecystectomy: A Randomized Double-Blind Study. Anesth Essays Res. 2019 Jan-Mar; 13(1): 97–104.
15.
Gülay EREN, Betül KOZANHAN, Oya HERGÜNSEL, Ünsal BİLGİN, Güray DEMİR, Zafer ÇUKUROVA. Pregabalin Blunts Cardiovascular Response to Laryngoscopy and Tracheal Intubation. Turkiye Klinikleri J Anest Reanim. 2009; 7(2): 82–7.
16.
Chakraborty R, Jain R, Sharma R. Evaluation of the efficacy of pre-operative oral pregabalin in attenuating hemodynamic response to laryngoscopy and intubation and on post-operative pain in patients undergoing elective surgery under general anaesthesia. Indian J Clin Anaesthe. 2016; 3: 419–26.
17.
Sundar AS, Kodali R, Sulaiman S, Ravullapalli H, Karthekeyan R, Vakamudi M, et al. The effects of preemptive pregabalin on attenuation of stress response to endotracheal intubation and opioid-sparing effect in patients undergoing off-pump coronary artery bypass grafting. Ann Card Anaesth. 2012; 15: 18–25.
18.
Saxena A, Gupta P, Chaudhary L. Effect of pregabalin premedication on the laryngoscopy response and intra-operative hemodynamic variables in laparoscopic cholecystectomy: A randomized comparison of two doses. Int J Sci Stud. 2016; 4: 75–80.
19.
Reuben SS, Buvanendran A, Kroin JS, Raghunathan K. The analgesic efficacy of celecoxib, pregabalin, and their combination for spinal fusion surgery. Anesth Analg. 2006; 103: 1271–1277.
20.
Spreng UJ, Dahl V, Raeder J. Effect of a single dose of pregabalin on post-operative pain and pre-operative anxiety in patients undergoing discectomy. Acta Anaesthesiol Scand. 2011; 55(5): 571–576.
21.
Kim SY, Song JW, Park B, Park S, An YJ, Shim YH. Pregabalin reduces post-operative pain after mastectomy: A double-blind, randomized, placebo-controlled study. Acta Anaesthesiol Scand. 2011; 55: 290–6.
22.
Baloyiannis I, Theodorou E, Sarakatsianou C, Stavroula G, Periyoliotis K, Tzovaras G. The effect of preemptive use of pregabalin on postoperative morphine consumption and analgesia levels after laparoscopic colorectal surgery: a controlled randomized trial. International Journal of Colorectal Disease. 2020; 35(2): 323.
23.
Warner FM, Cragg JJ, Jutzeler CR, Röhrich F, Weidner N, Saur M, Maier DD, Schuld C; EMSCI Sites, Curt A, Kramer JK. Early Administration of Gabapentinoids Improves Motor Recovery after Human Spinal Cord Injury. Cell Rep. 2017 Feb 14; 18(7): 1614–1618.
24.
Hu J, Huang D, Li M, Wu C, Zhang J. Effects of a single dose of preoperative pregabalin and gabapentin for acute postoperative pain: a network meta-analysis of randomized controlled trials. J Pain Res. 2018; 11: 2633–2643.
25.
Prasoon Gupta, Anudeep Saxena, Lalita Chaudhary. Effect of Pregabalin Premedication on the Requirement of Anesthetic and Analgesic Drugs in Laparoscopic Cholecystectomy: Randomized Comparison of Two Doses. Anesth Essays Res. 2017 Apr-Jun; 11(2): 330–333.
26.
Rajappa GC, Vig S, Bevanaguddaiah Y, Anadaswamy TC. Efficacy of Pregabalin as Premedication for Post-Operative Analgesia in Vaginal Hysterectomy. Anesth Pain Med. 2016; 6(3): e34591.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.