REVIEW PAPER
Etiology, symptoms and treatment of peri-menopausal depression
1
Medical University of Silesia, Katowice, Poland
2
Department Pathophysiology and Endocrinology Medical University of Silesia, Katowice, Poland
3
Student Scientific Circle at the Department of Psychiatry, Medical University of Silesia, Katowice, Poland
J Pre Clin Clin Res. 2023;17(2):91-94
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Menopause is associated with the onset of a variety of symptoms that have a significant impact on a woman’s daily functioning. Many women develop depressive disorders as their hormone levels fluctuate and their stress response pathways change. The goal of this study was to collect up-to-date information on the etiology, symptoms, and treatment of peri-menopausal depression.
Review methods:
PubMed and Google Scholar databases were searched for articles on menopausal women’s mental health published between 1991 and 2022. Ninety articles were discovered and categorized by content and topic. The 35 most pertinent and current articles were selected.
Brief description of the state of knowledge:
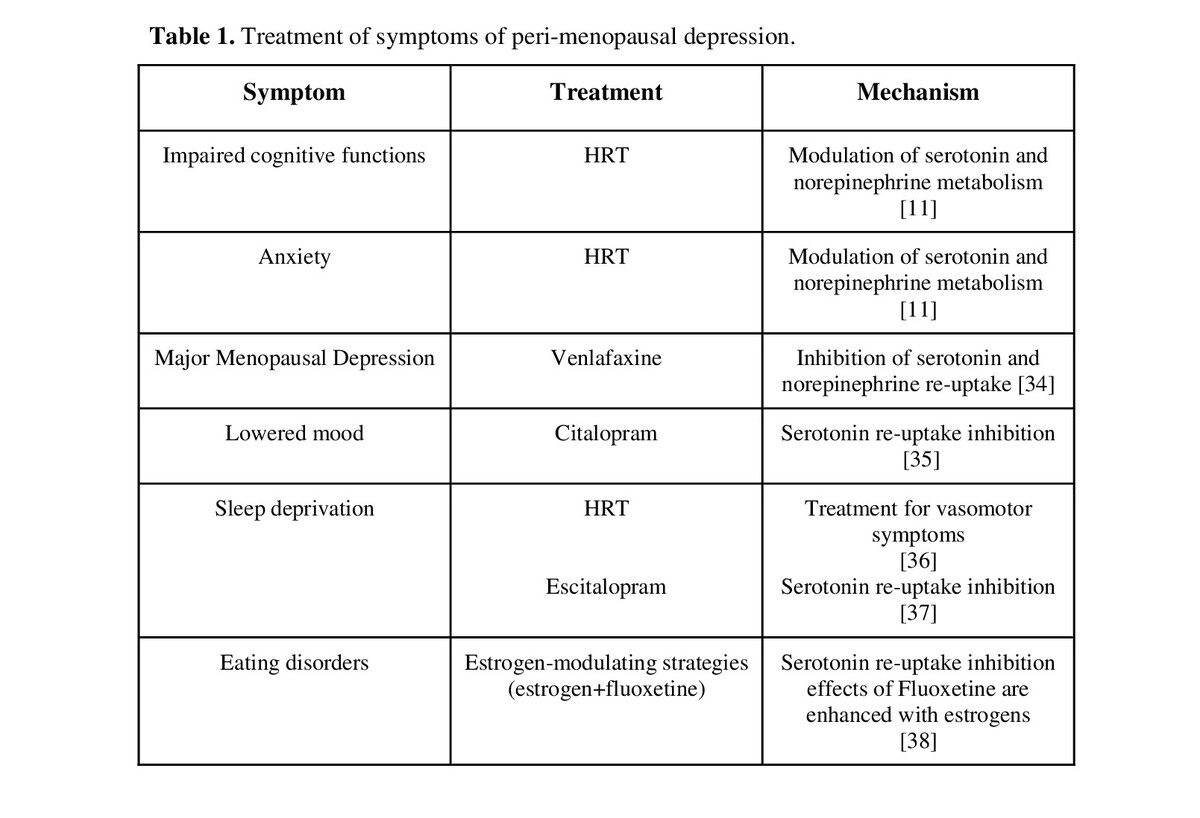
According to a review of the literature, major depressive disorders are most common in women during the menopausal transition due to hormonal fluctuations which are at their peak. This is because previously unknown negative menopausal symptoms have emerged, such as sleep disturbances, hot flashes, excessive sweating, weight gain, and mood disorders.
Summary:
Women with a proclivity for depressive behavior and a lower level of education are more likely to develop more severe psychiatric symptoms. Adequate pharmacotherapy, as well as prevention in the form of regular exercise and psychotherapy, should be implemented early in the development of mood disorders. In addition to implementing pharmacotherapy, women going through menopause should be encouraged to exercise and receive psychological counseling.
Menopause is associated with the onset of a variety of symptoms that have a significant impact on a woman’s daily functioning. Many women develop depressive disorders as their hormone levels fluctuate and their stress response pathways change. The goal of this study was to collect up-to-date information on the etiology, symptoms, and treatment of peri-menopausal depression.
Review methods:
PubMed and Google Scholar databases were searched for articles on menopausal women’s mental health published between 1991 and 2022. Ninety articles were discovered and categorized by content and topic. The 35 most pertinent and current articles were selected.
Brief description of the state of knowledge:
According to a review of the literature, major depressive disorders are most common in women during the menopausal transition due to hormonal fluctuations which are at their peak. This is because previously unknown negative menopausal symptoms have emerged, such as sleep disturbances, hot flashes, excessive sweating, weight gain, and mood disorders.
Summary:
Women with a proclivity for depressive behavior and a lower level of education are more likely to develop more severe psychiatric symptoms. Adequate pharmacotherapy, as well as prevention in the form of regular exercise and psychotherapy, should be implemented early in the development of mood disorders. In addition to implementing pharmacotherapy, women going through menopause should be encouraged to exercise and receive psychological counseling.
Gębka NM, Głogowska-Szeląg J, Gębka D, Adamczyk J. Etiology, symptoms and treatment of peri-menopausal depression. J Pre-Clin Clin Res.
2023; 17(2): 91–94. doi: 10.26444/jpccr/162920
REFERENCES (38)
1.
Abdel-Salam DM, Mohamed RA, Alruwaili RR, Alhablani FS, Aldaghmi RM, ALghassab RE. Postmenopausal Symptoms and Their Correlates among Saudi Women Attending Different Primary Health Centers. Int J Environ Res Public Health. 2021;18(13):6831. doi:10.3390/ijerph18136831.
2.
Ali AM, Ahmed AH, Smail L. Psychological Climacteric Symptoms and Attitudes toward Menopause among Emirati Women. Int J Environ Res Public Health. 2020;17(14):5028. doi:10.3390/ijerph17145028.
3.
Inayat K, Danish N, Hassan L. Symptoms Of Menopause In Peri And Postmenopausal Women And Their Attitude Towards Them. J Ayub Med Coll Abbottabad. 2017;29(3):477–480.
4.
Gordon JL, Sander B, Eisenlohr-Moul TA, Sykes Tottenham L. Mood sensitivity to estradiol predicts depressive symptoms in the menopause transition. Psychol Med. 2021;51(10):1733–1741. doi:10.1017/S0033291720000483.
5.
Dotlic J, Radovanovic S, Rancic B, Milosevic B, Nicevic S, Kurtagic I, Markovic N, Gazibara T. Mental health aspect of quality of life in the menopausal transition. J Psychosom Obstet Gynaecol. 2021;42(1):40–49.doi:10.1080/0167482X.2020.1734789.
6.
Campbell KE, Szoeke CE, Dennerstein L. The course of depressive symptoms during the postmenopause: a review. Womens Midlife Health. 2015;1:3. doi:10.1186/s40695-015-0003-x.
7.
Campbell KE, Dennerstein L, Finch S, Szoeke CE. Impact of menopausal status on negative mood and depressive symptoms in a longitudinal sample spanning 20 years. Menopause. 2017;24(5):490–496. doi:10.1097/GME.0000000000000805.
8.
Gordon JL, Girdler SS, Meltzer-Brody SE, Stika CS, Thurston RC, Clark CT, Prairie BA, Moses-Kolko E, Joffe H, Wisner KL. Ovarian hormone fluctuation, neurosteroids, and HPA axis dysregulation in perimenopausal depression: a novel heuristic model. Am J Psychiatry. 2015;172(3):227–36. doi:10.1176/appi.ajp.2014.14070918.
9.
de Kruif M, Spijker AT, Molendijk ML. Depression during the perimenopause: A meta-analysis. J Affect Disord. 2016;206:174–180. doi:10.1016/j.jad.2016.07.040.
10.
Hall MH, Kline CE, Nowakowski S. Insomnia and sleep apnea in midlife women: prevalence and consequences to health and functioning. F1000Prime Rep. 2015;7:63. doi: 10.12703/P7-63.
11.
Birkhäuser M. Depressionen und Angstzustände im Klimakterium [Climacteric depression and anxiety]. Ther Umsch. 2021;78(8):427–434. doi:10.1024/0040-5930/a001293.
12.
Ryan J, Burger HG, Szoeke C, Lehert P, Ancelin ML, Henderson VW, Dennerstein L. A prospective study of the association between endogenous hormones and depressive symptoms in postmenopausal women. Menopause. 2009;16(3):509–17. doi:10.1097/gme.0b013e31818d635f.
13.
Santoro N, Roeca C, Peters BA, Neal-Perry G. The Menopause Transition: Signs, Symptoms, and Management Options. J Clin Endocrinol Metab. 2021;106(1):1–15. doi:10.1210/clinem/dgaa764.
14.
Mulhall S, Andel R, Anstey KJ. Variation in symptoms of depression and anxiety in midlife women by menopausal status. Maturitas. 2018;108:7–12.
15.
Cao H, Li S, Baranova A, Zhang F. Shared Genetic Liability Between Major Depressive Disorder and Atopic Diseases. Front Immunol. 2021;12:665160. doi:10.3389/fimmu.2021.665160.
16.
Maki PM, Kornstein SG, Joffe H, Bromberger JT, Freeman EW, Athappilly G, Bobo WV, Rubin LH, Koleva HK, Cohen LS, Soares CN. Guidelines for the Evaluation and Treatment of Perimenopausal Depression: Summary and Recommendations. J Womens Health (Larchmt). 2019;28(2):117–134. doi:10.1089/jwh.2018.27099.mensocrec.
17.
Eskola PJ, Jokelainen J, Järvelin MR, Keinänen-Kiukaanniemi S, Ruokonen A, Puukka K, Timonen M, Auvinen JP. Depression and Insulin Resistance: Additional Support for the Novel Heuristic Model in Perimenopausal Depression. Am J Psychiatry. 2015;172(8):796–7. doi:10.1176/appi.ajp.2015.15030377.
18.
Balan I, Aurelian L, Williams KS, Campbell B, Meeker RB, Morrow AL. Inhibition of human macrophage activation via pregnane neurosteroid interactions with toll-like receptors: Sex differences and structural requirements. Front Immunol. 2022;13:940095. doi:10.3389/fimmu.2022.940095.
19.
Hernandez GD, Brinton RD. Allopregnanolone: Regenerative therapeutic to restore neurological health. Neurobiol Stress. 2022;21:100502. doi:10.1016/j.ynstr.2022.100502.
20.
Hantsoo L, Duffy KA, Sammel M, Johnson RL, Kim D, Grillon C, Epperson CN. Enduring impact of childhood adversity: Affective modulation of acoustic startle response during pregnancy and postpartum. Physiol Behav. 2023;258:114031. doi:10.1016/j.physbeh.2022.114031.
21.
Pluchino N, Cubeddu A, Giannini A, Merlini S, Cela V, Angioni S, Genazzani A. Progestogens and brain: an update. Maturitas. 2009;62(4):349–55.
22.
Purdy RH, Morrow AL, Moore PH, Paul SM. Stress-induced elevations of gamma-aminobutyric acid type A receptor-active steroids in the rat brain. Proceedings of the National Academy of Sciences. 1991;88(10):4553–7.
23.
Verbe J, Dubertret C, El-Hage W, Bonnet-Brilhault F, Duriez P. Approche GABAergique de la dépression du post-partum: une revue critique translationnelle [GABAergic approach of postpartum depression: A translational review of literature]. Encephale. 2020;46(2):123–134. doi:10.1016/j.encep.2019.09.007.
24.
Shen H, Gong QH, Aoki C, Yuan M, Ruderman Y, Dattilo M, Williams K, Smith SS. Reversal of neurosteroid effects at α4β2δ GABAA receptors triggers anxiety at puberty. Nature Neuroscience. 2007;10(4):469–77.
25.
Gilfarb RA, Leuner B. GABA System Modifications During Periods of Hormonal Flux Across the Female Lifespan. Front Behav Neurosci. 2022;16:802530. doi: 10.3389/fnbeh.2022.802530.
26.
Bixo M, Johansson M, Timby E, Michalski L, Bäckström T. Effects of GABA active steroids in the female brain with a focus on the premenstrual dysphoric disorder. J Neuroendocrinol. 2018;30(2). doi:10.1111/jne.12553.
27.
Iwata S, Wakita M, Shin M-C, Fukuda A, Akaike N. Modulation of allopregnanolone on excitatory transmitters release from single glutamatergic terminal. Brain research bulletin. 2013;93:39–46. [PubMed: 23174309].
28.
Sanacora G, Treccani G, Popoli M. Towards a glutamate hypothesis of depression: an emerging frontier of neuropsychopharmacology for mood disorders. Neuropharmacology. 2012;62(1):63–77. [PubMed: 21827775].
29.
Chandankhede M, Gupta M, Pakhmode S. Assessment of Psychological Status and Oxidative Stress in Postmenopausal Women: A Cross-Sectional Study. J Menopausal Med. 2021;27(3):155–161. doi:10.6118/jmm.20035.
30.
Gordon JL, Rubinow DR, Eisenlohr-Moul TA, Xia K, Schmidt PJ, Girdler SS. Efficacy of Transdermal Estradiol and Micronized Progesterone in the Prevention of Depressive Symptoms in the Menopause Transition: A Randomized Clinical Trial. JAMA Psychiatry. 2018;75(2):149–157. doi:10.1001/jamapsychiatry.2017.3998.
31.
Soares CN, Almeida OP, Joffe H, Cohen LS. Efficacy of estradiol for the treatment of depressive disorders in perimenopausal women: a double-blind, randomized, placebo-controlled trial. Archives of General Psychiatry. 2001;58(June (6)):529–34.
32.
Wium-Andersen MK, Jørgensen TSH, Halvorsen AH, Hartsteen BH, Jørgensen MB, Osler M. Association of Hormone Therapy With Depression During Menopause in a Cohort of Danish Women. JAMA Netw Open. 2022;5(11):e2239491. doi:10.1001/jamanetworkopen.2022.39491.
33.
Soares CN. Depression and Menopause: Current Knowledge and Clinical Recommendations for a Critical Window. Psychiatr Clin North Am. 2017;40(2):239–254. doi:10.1016/j.psc.2017.01.007.
34.
Zhou J, Wang X, Feng L, Xiao L, Yang R, Zhu X, Shi H, Hu Y, Chen R, Boyce P, Wang G. Venlafaxine vs. fluoxetine in postmenopausal women with major depressive disorder: an 8-week, randomized, single-blind, active-controlled study. BMC Psychiatry. 2021;21(1):260. doi: 10.1186/s12888-021-03253-8.
35.
Qi Q, Zhang X, Yao L, Chen Y, Weng H. Pueratin improves diminished ovarian reserve by inhibiting apoptosis. Exp Ther Med. 2021;22(6):1423. doi:10.3892/etm.2021.10858.
36.
Baker FC, de Zambotti M, Colrain IM, Bei B. Sleep problems during the menopausal transition: prevalence, impact, and management challenges. Nat Sci Sleep. 2018;10:73–95. doi:10.2147/NSS.S125807.
37.
Attarian H, Hachul H, Guttuso T, Phillips B. Treatment of chronic insomnia disorder in menopause: evaluation of literature. Menopause. 2015;22(6):674–684.
38.
Baker JH, Runfola CD. Eating disorders in midlife women: A perimenopausal eating disorder? Maturitas. 2016;85:112–6. doi:10.1016/j.maturitas.2015.12.017.
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.