REVIEW PAPER
Current knowledge of PANDAS and PANS syndromes in paediatric patients – etiology, diagnosis and therapies
1
III Faculty of Paediatrics, Medical University, Lublin, Poland
2
III Faculty of Paediatrics, Clinic of Paediatric Neurology, Medical University, Lublin, Poland
J Pre Clin Clin Res. 2024;18(4):324-332
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
PANDAS (Paediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections) and PANS (Paediatric Acute-onset Neuropsychiatric Syndrome) are rare diseases and there is scant information about diagnostic and treatment options. The aim of this study is to summarise the current state of knowledge about the diseases.
Review methods:
Articles from the PubMed database were sought and articles found dealing with the diseases were summarised and the knowledge assessed.
Brief description of the state of knowledge:
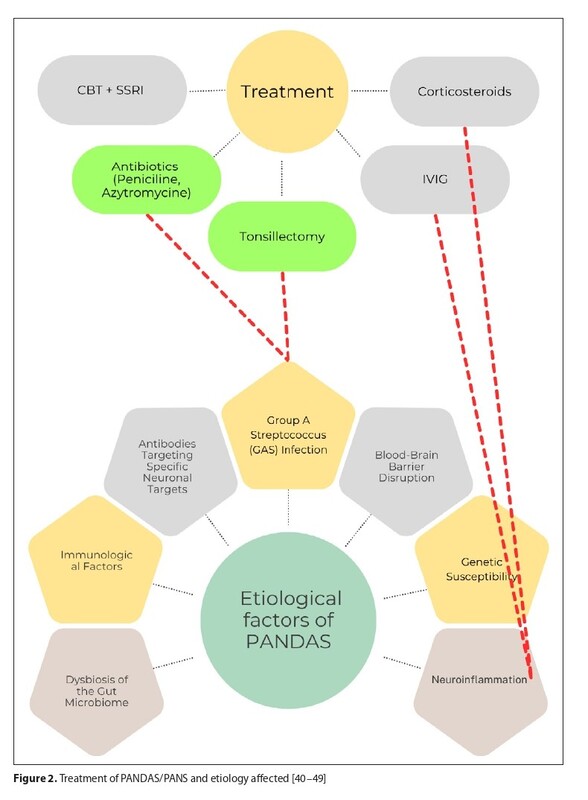
The etiology of PANDAS and PANS syndromes has not yet been defined. There are hypotheses assuming that streptococcal infection can trigger an immune response that results in prominent neuropsychiatric symptoms. Diagnostic criteria focus on a clinical picture that includes the sudden onset of tics, obsessivecompulsive behaviour, anxiety and mood disorders following infection. Therapy for PANDAS and PANS syndromes is based at present on a number of therapeutic avenues for selecting the best plan. Immunomodulatory therapies, such as plasmapheresis and immunoglobulin administration, are being explored as methods to reduce the severity of the intractable symptoms in children. In addition, behavioural and pharmacological therapies, such as antipsychotics or anticonvulsants, are being used to manage symptoms.
Summary:
Despite the clear interest in understanding these syndromes, there is a need for further research, especially in the area of identifying pathomechanisms and optimal treatment strategies. Improving diagnostic and therapeutic processes will ensure faster recovery and prevention of these conditions in paediatric patients in the interest of their well-being and comfort.
PANDAS (Paediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections) and PANS (Paediatric Acute-onset Neuropsychiatric Syndrome) are rare diseases and there is scant information about diagnostic and treatment options. The aim of this study is to summarise the current state of knowledge about the diseases.
Review methods:
Articles from the PubMed database were sought and articles found dealing with the diseases were summarised and the knowledge assessed.
Brief description of the state of knowledge:
The etiology of PANDAS and PANS syndromes has not yet been defined. There are hypotheses assuming that streptococcal infection can trigger an immune response that results in prominent neuropsychiatric symptoms. Diagnostic criteria focus on a clinical picture that includes the sudden onset of tics, obsessivecompulsive behaviour, anxiety and mood disorders following infection. Therapy for PANDAS and PANS syndromes is based at present on a number of therapeutic avenues for selecting the best plan. Immunomodulatory therapies, such as plasmapheresis and immunoglobulin administration, are being explored as methods to reduce the severity of the intractable symptoms in children. In addition, behavioural and pharmacological therapies, such as antipsychotics or anticonvulsants, are being used to manage symptoms.
Summary:
Despite the clear interest in understanding these syndromes, there is a need for further research, especially in the area of identifying pathomechanisms and optimal treatment strategies. Improving diagnostic and therapeutic processes will ensure faster recovery and prevention of these conditions in paediatric patients in the interest of their well-being and comfort.
Zych K, Burdan O, Ziomek WN, Białek AB, Wróbel J, Cieślik-Porębska M, Urbańska S, Chrościńska-Krawczyk M. Current knowledge of PANDAS and
PANS syndromes in paediatric patients: etiology, diagnosis and therapies. J Pre-Clin Clin Res. 2024; 18(4): 324–332. doi: 10.26444/jpccr/193989
REFERENCES (56)
1.
Wald ER, Eickhoff J, Flood GE, et al. Estimate of the incidence of PANDAS and PANS in 3 primary care populations. Front Pediatr. 2023;11:1170379. https://doi.org/10.3389/fped.2....
2.
Wilbur C, Bitnun A, Kronenberg S, et al. PANDAS/PANS in childhood: Controversies and evidence. Paediatr Child Health. 2019;24(2):85–91. https://doi.org/10.1093/pch/px....
3.
Prato A, Gulisano M, Scerbo M, et al. Diagnostic Approach to Pediatric Autoimmune Neuropsychiatric Disorders Associated With Streptococcal Infections (PANDAS): A Narrative Review of Literature Data. Front Pediatr. 2021;9:746639. https://doi.org/10.3389/fped.2....
4.
Sigra S, Hesselmark E, Bejerot S. Treatment of PANDAS and PANS: a systematic review. Neurosci Biobehav Rev. 2018;86:51–65. https://doi.org/10.1016/j.neub....
5.
Singer HS, Gilbert DL, Wolf DS, et al. Moving from PANDAS to CANS. J Pediatr. 2012;160(5):725–731. https://doi.org/10.1016/j.jped....
6.
La Bella S, Scorrano G, Rinaldi M, et al. Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections (PANDAS): Myth or Reality? The State of the Art on a Controversial Disease. Microorganisms. 2023;11(10):2549. https://doi.org/10.3390/microo....
7.
Blum K, Dennen CA, Braverman ER, et al. Hypothesizing That Pediatric Autoimmune Neuropsychiatric Associated Streptococcal (PANDAS) Causes Rapid Onset of Reward Deficiency Syndrome (RDS) Behaviors and May Require Induction of “Dopamine Homeostasis”. Open J Immunol. 2022;12(3):65–75. https://doi.org/10.4236/oji.20....
8.
Xu J, Liu RJ, Fahey S, et al. Antibodies From Children With PANDAS Bind Specifically to Striatal Cholinergic Interneurons and Alter Their Activity. Am J Psychiatry. 2021;178(1):48–64. https://doi.org/10.1176/appi.a....
9.
Zheng J, Frankovich J, McKenna ES, et al. Association of Pediatric Acute-Onset Neuropsychiatric Syndrome With Microstructural Differences in Brain Regions Detected via Diffusion-Weighted Magnetic Resonance Imaging. JAMA Netw Open. 2020;3(5). https://doi.org/10.1001/jamane....
10.
Frick LR, Rapanelli M, Jindachomthong K, et al. Differential binding of antibodies in PANDAS patients to cholinergic interneurons in the striatum. Brain Behav Immun. 2018;69:304–311. https://doi.org/10.1016/j.bbi.....
11.
Hutanu A, Reddy LN, Mathew J, et al. Pediatric Autoimmune Neuropsychiatric Disorders Associated With Group A Streptococci: Etiopathology and Diagnostic Challenges. Cureus. 2022;14(8). https://doi.org/10.7759/cureus....
12.
Quagliariello A, Del Chierico F, Russo A, et al. Gut Microbiota Profiling and Gut-Brain Crosstalk in Children Affected by Pediatric Acute-Onset Neuropsychiatric Syndrome and Pediatric Autoimmune Neuropsychiatric Disorders Associated With Streptococcal Infections. Front Microbiol. 2018;9:675. https://doi.org/10.3389/fmicb.....
13.
Baj J, Sitarz E, Forma A, et al. Alterations in the Nervous System and Gut Microbiota after β-Hemolytic Streptococcus Group A Infection-Characteristics and Diagnostic Criteria of PANDAS Recognition. Int J Mol Sci. 2020;21(4):1476. https://doi.org/10.3390/ijms21....
14.
Dop D, Marcu IR, Padureanu R, et al. Pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections (Review). Exp Ther Med. 2021;21(1):94. https://doi.org/10.3892/etm.20....
15.
Orefici G, Cardona F, Cox CJ, et al. Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections (PANDAS). In: Ferretti JJ, editor. Streptococcus pyogenes: Basic Biology to Clinical Manifestations. University of Oklahoma Health Sciences Center; 2016. PMID: 26866234.
16.
Windfuhr JP. Tonsillectomy remains a questionable option for pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections (PANDAS). GMS Curr Top Otorhinolaryngol Head Neck Surg. 2016;15. https://doi.org/10.3205/cto000....
17.
Toufexis MD, Hommer R, Gerardi DM, et al. Disordered eating and food restrictions in children with PANDAS/PANS. J Child Adolesc Psychopharmacol. 2015;25(1):48–56. https://doi.org/10.1089/cap.20....
18.
Swedo SE, Seidlitz J, Kovacevic M, et al. Clinical presentation of pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections in research and community settings. J Child Adolesc Psychopharmacol. 2015;25(1):26–30. https://doi.org/10.1089/cap.20....
19.
Prosell U, Norman H, Sand A, et al. Infection and speech: Disfluency and other speech symptoms in Pediatric Acute-onset Neuropsychiatric Syndrome. J Commun Disord. 2022;99:106250. https://doi.org/10.1016/j.jcom....
20.
Masterson EE, Gavin JM. Baseline characteristics of children in the International PANS Registry (IPR) Epidemiology Study. BMJ Open. 2024;14(1). https://doi.org/10.1136/bmjope....
21.
Krouse A, Li H, Krenzer JA, et al. Plasmapheresis, Rituximab, and Ceftriaxone Provided Lasting Improvement for a 27-Year-Old Adult Male with Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections (PANDAS). Case Rep Psychiatry. 2021;2021:8697902. https://doi.org/10.1155/2021/8....
22.
Teixeira AL, Vasconcelos LP, Nunes MDCP, et al. Sydenham’s chorea: from pathophysiology to therapeutics. Expert Rev Neurother. 2021;21(8):913–922. https://doi.org/10.1080/147371....
23.
Meyer J. Inflammation, Obsessive-Compulsive Disorder, and Related Disorders. Curr Top Behav Neurosci. 2021;49:31–53. https://doi.org/10.1007/7854_2....
24.
Pérez-Vigil A, Fernández de la Cruz L, Brander G, et al. The link between autoimmune diseases and obsessive-compulsive and tic disorders: A systematic review. Neurosci Biobehav Rev. 2016;71:542–562. https://doi.org/10.1016/j.neub....
25.
Orlovska S, Vestergaard CH, Bech BH, et al. Association of Streptococcal Throat Infection With Mental Disorders: Testing Key Aspects of the PANDAS Hypothesis in a Nationwide Study. JAMA Psychiatry. 2017;74(7):740–746. https://doi.org/10.1001/jamaps....
26.
Hsu CJ, Wong LC, Lee WT. Immunological Dysfunction in Tourette Syndrome and Related Disorders. Int J Mol Sci. 2021;22(2):853. https://doi.org/10.3390/ijms22....
27.
Singh R, Nekrasova N, Butov D. Tourette syndrome or PANDAS-a case report. Wien Med Wochenschr. 2021;171(11–12):289–292. https://doi.org/10.1007/s10354....
28.
Church AJ, Dale RC, Lees AJ, et al. Tourette’s syndrome: a cross sectional study to examine the PANDAS hypothesis. J Neurol Neurosurg Psychiatry. 2003;74(5):602–607. https://doi.org/10.1136/jnnp.7....
29.
van Toorn R, Weyers HH, Schoeman JF. Distinguishing PANDAS from Sydenham’s chorea: case report and review of the literature. Eur J Paediatr Neurol. 2004;8(4):211–216. https://doi.org/10.1016/j.ejpn....
30.
Pankratz B, Feige B, Runge K, et al. Cerebrospinal fluid findings in patients with obsessive-compulsive disorder, Tourette syndrome, and PANDAS: A systematic literature review. Brain Behav Immun. 2024;115:319–332. https://doi.org/10.1016/j.bbi.....
31.
Gamucci A, Uccella S, Sciarretta L, et al. PANDAS and PANS: Clinical, Neuropsychological, and Biological Characterization of a Monocentric Series of Patients and Proposal for a Diagnostic Protocol. J Child Adolesc Psychopharmacol. 2019;29(4):305–312. https://doi.org/10.1089/cap.20....
32.
La Bella S, Attanasi M, Di Ludovico A, et al. Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections (PANDAS) Syndrome: A 10-Year Retrospective Cohort Study in an Italian Centre of Pediatric Rheumatology. Microorganisms. 2023;12(1):8. https://doi.org/10.3390/microo....
33.
Endres D, Pollak TA, Bechter K, et al. Immunological causes of obsessive-compulsive disorder: is it time for the concept of an “autoimmune OCD” subtype?. Transl Psychiatry. 2022;12(1):5. https://doi.org/10.1038/s41398....
34.
Chang K, Frankovich J, Cooperstock M, et al. Clinical evaluation of youth with pediatric acute-onset neuropsychiatric syndrome (PANS): recommendations from the 2013 PANS Consensus Conference. J Child Adolesc Psychopharmacol. 2015;25(1):3–13. https://doi.org/10.1089/cap.20....
35.
Vreeland A, Calaprice D, Or-Geva N, et al. Postinfectious Inflammation, Autoimmunity, and Obsessive-Compulsive Disorder: Sydenham Chorea, Pediatric Autoimmune Neuropsychiatric Disorder Associated with Streptococcal Infection, and Pediatric Acute-Onset Neuropsychiatric Disorder. Dev Neurosci. 2023;45(6):361–374. https://doi.org/10.1159/000534....
36.
Thienemann M, Murphy T, Leckman J, et al. Clinical Management of Pediatric Acute-Onset Neuropsychiatric Syndrome: Part I-Psychiatric and Behavioral Interventions. J Child Adolesc Psychopharmacol. 2017;27(7):566–573. https://doi.org/10.1089/cap.20....
37.
Wells L, O’Hara N, Frye RE, et al. Folate Receptor Alpha Autoantibodies in the Pediatric Acute-Onset Neuropsychiatric Syndrome (PANS) and Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections (PANDAS) Population. J Pers Med. 2024;14(2):166. https://doi.org/10.3390/jpm140....
38.
Hesselmark E, Bejerot S. Biomarkers for diagnosis of Pediatric Acute Neuropsychiatric Syndrome (PANS) – Sensitivity and specificity of the Cunningham Panel. J Neuroimmunol. 2017;312:31–37. https://doi.org/10.1016/j.jneu....
39.
Hesselmark E, Bejerot S. Patient Satisfaction and Treatments Offered to Swedish Patients with Suspected Pediatric Acute-Onset Neuropsychiatric Syndrome and Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections. J Child Adolesc Psychopharmacol. 2019;29(8):634–641. https://doi.org/10.1089/cap.20....
40.
Chiarello F, Spitoni S, Hollander E, et al. An expert opinion on PANDAS/PANS: highlights and controversies. Int J Psychiatry Clin Pract. 2017;21(2):91–98. https://doi.org/10.1080/136515....
41.
Burchi E, Pallanti S. Antibiotics for PANDAS? Limited Evidence: Review and Putative Mechanisms of Action. Prim Care Companion CNS Disord. 2018;20(3):17r02232. https://doi.org/10.4088/PCC.17....
42.
Snider LA, Lougee L, Slattery M, et al. Antibiotic prophylaxis with azithromycin or penicillin for childhood-onset neuropsychiatric disorders. Biol Psychiatry. 2005;57(7):788–792. https://doi.org/10.1016/j.biop....
43.
Demesh D, Virbalas JM, Bent JP. The role of tonsillectomy in the treatment of pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections (PANDAS). JAMA Otolaryngol Head Neck Surg. 2015;141(3):272–275. https://doi.org/10.1001/jamaot....
44.
Frankovich J, Swedo S, Murphy T, et al. Clinical Management of Pediatric Acute-Onset Neuropsychiatric Syndrome: Part II-Use of Immunomodulatory Therapies. J Child Adolesc Psychopharmacol. 2017;27(7):574–593. https://doi.org/10.1089/cap.20....
45.
Brown K, Farmer C, Farhadian B, et al. Pediatric Acute-Onset Neuropsychiatric Syndrome Response to Oral Corticosteroid Bursts: An Observational Study of Patients in an Academic Community-Based PANS Clinic. J Child Adolesc Psychopharmacol. 2017;27(7):629–639. https://doi.org/10.1089/cap.20....
46.
Latimer ME, L’Etoile N, Seidlitz J, et al. Therapeutic plasma apheresis as a treatment for 35 severely ill children and adolescents with pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections. J Child Adolesc Psychopharmacol. 2015;25(1):70–75. https://doi.org/10.1089/cap.20....
47.
Prus K, Weidner K, Alquist C. Therapeutic plasma exchange in adolescent and adult patients with autoimmune neuropsychiatric disorders associated with streptococcal infections. J Clin Apher. 2022;37(6):597–599. https://doi.org/10.1002/jca.22....
48.
Eremija J, Patel S, Rice S, et al. Intravenous immunoglobulin treatment improves multiple neuropsychiatric outcomes in patients with pediatric acute-onset neuropsychiatric syndrome. Front Pediatr. 2023;11:1229150. https://doi.org/10.3389/fped.2....
49.
Williams KA, Swedo SE, Farmer CA, et al. Randomized, Controlled Trial of Intravenous Immunoglobulin for Pediatric Autoimmune Neuropsychiatric Disorders Associated With Streptococcal Infections. J Am Acad Child Adolesc Psychiatry. 2016;55(10):860–867.e2. https://doi.org/10.1016/j.jaac....
50.
Pallanti S, Di Ponzio M. PANDAS/PANS in the COVID-19 Age: Autoimmunity and Epstein-Barr Virus Reactivation as Trigger Agents?. Children. 2023;10(4):648. https://doi.org/10.3390/childr....
51.
Marazziti D, Palermo S, Arone A, et al. Obsessive-Compulsive Disorder, PANDAS, and Tourette Syndrome: Immuno-inflammatory Disorders. In: Advances in Experimental Medicine and Biology. Singapore: Springer; 2023. p. 275–300. https://doi.org/10.1007/978-98....
52.
Bransfield RC, Mao C, Greenberg R. Microbes and Mental Illness: Past, Present, and Future. Healthcare (Basel). 2023;12(1):83. https://doi.org/10.3390/health....
53.
Gagliano A, Carta A, Tanca MG, et al. Pediatric Acute-Onset Neuropsychiatric Syndrome: Current Perspectives. Neuropsychiatr Dis Treat. 2023;19:1221–1250. https://doi.org/10.2147/NDT.S3....
54.
Nazeer A, Latif F, Mondal A, et al. Obsessive-compulsive disorder in children and adolescents: epidemiology, diagnosis and management. Transl Pediatr. 2020;9(Suppl 1). https://doi.org/10.21037/tp.20....
55.
Tang AW, Appel HJ, Bennett SC, et al. Treatment barriers in PANS/PANDAS: Observations from eleven health care provider families. Fam Syst Health. 2021;39(3):477–487. https://doi.org/10.1037/fsh000....
56.
Murphy TK, Gerardi DM, Leckman JF. Pediatric acute-onset neuropsychiatric syndrome. Psychiatr Clin North Am. 2014;37(3):353–374. https://doi.org/10.1016/j.psc.....
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.