RESEARCH PAPER
Comparison of Peak Expiratory Flow Rates (PEFR) between obese and non-obese Females
1
Thanjavur Medical College, India
J Pre Clin Clin Res. 2021;15(3):111-115
KEYWORDS
TOPICS
ABSTRACT
Introduction:
In India, obesity is rapidly escalating in all age groups. Obesity has significant effects on respiratory function and reduces lung volume. Peak Expiratory Flow Rate (PEFR) demonstrates the calibre of the airways and is accepted worldwide as the objective indicator of ventilatory capacity, and is useful for the diagnosis and management of respiratory illness. Objective. The aim of this study was to compare the Peak Expiratory Flow Rates between obese and non-obese females aged 35–45.
Material and methods:
40 healthy obese females with BMI ≥30Kg/m2 and 40 healthy non-obese females with BMI (18.5–24.9 Kg/m2) as controls were included in the study. Subjects with H/o cardiopulmonary illness, asthma, diabetes mellitus, hypertension, smokers, on chronic medication, subjects who had noticeable weight gain / loss over the preceding 3 months, were all excluded. PEFR Measurements were performed using a Mini Wright’s Peak Flow Meter. Three readings at 2 minutes intervals were recorded. The maximum of the 3 values were taken as the PEFR. The results were statistically analysed using Students Unpaired t- test
Results:
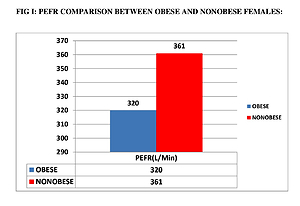
PEFR in obese females (320±28.06 L/Min) was significantly lower than the non-obese females (361±29.17L/Min), which was statistically significant (p=0.000; p<0.05). PEFR was negatively correlated with BMI (Pearson’s correlation r = -.127) significant at p<0.01 level.
Conclusions:
There occurs a significant reduction in PEFR in obese females, compared to non-obese females. This study highlights the need for aggressive reduction of weight in obese females in order to increase respiratory efficiency
In India, obesity is rapidly escalating in all age groups. Obesity has significant effects on respiratory function and reduces lung volume. Peak Expiratory Flow Rate (PEFR) demonstrates the calibre of the airways and is accepted worldwide as the objective indicator of ventilatory capacity, and is useful for the diagnosis and management of respiratory illness. Objective. The aim of this study was to compare the Peak Expiratory Flow Rates between obese and non-obese females aged 35–45.
Material and methods:
40 healthy obese females with BMI ≥30Kg/m2 and 40 healthy non-obese females with BMI (18.5–24.9 Kg/m2) as controls were included in the study. Subjects with H/o cardiopulmonary illness, asthma, diabetes mellitus, hypertension, smokers, on chronic medication, subjects who had noticeable weight gain / loss over the preceding 3 months, were all excluded. PEFR Measurements were performed using a Mini Wright’s Peak Flow Meter. Three readings at 2 minutes intervals were recorded. The maximum of the 3 values were taken as the PEFR. The results were statistically analysed using Students Unpaired t- test
Results:
PEFR in obese females (320±28.06 L/Min) was significantly lower than the non-obese females (361±29.17L/Min), which was statistically significant (p=0.000; p<0.05). PEFR was negatively correlated with BMI (Pearson’s correlation r = -.127) significant at p<0.01 level.
Conclusions:
There occurs a significant reduction in PEFR in obese females, compared to non-obese females. This study highlights the need for aggressive reduction of weight in obese females in order to increase respiratory efficiency
ACKNOWLEDGEMENTS
The authors express their thanks to all the participants and the technical personnel involved in this study.
FUNDING
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. The authors and planners have disclosed no potential conflicts of interest, financial or otherwise.
Shanmugapriya C, Vinodha R. Comparison of Peak Expiratory Flow Rates (PEFR) between Obese and Nonobese Females. J Pre-Clin Clin Res.
2021; 15(3): 111–115. doi: 10.26444/jpccr/139199
REFERENCES (20)
1.
Ramezankhany A, Nazar Ali P, Hedayati M. Comparing Effects of Aerobics, Pilates Exercises and Low Calorie Diet on Leptin Levels and Lipid Profiles in Sedentary Women. Iranian Journal of Basic Medical Sciences. 2011; 14(3): 256–263. doi: 10.22038/ijbms.2011.5003.
2.
Geissler C, Powers H. Human Nutrition. 12th ed. Edinburg: Elsevier Saunders; 2011. p. 401–423.
3.
Mengistie AB, Reddy RC, SyamBabu M. The effects of combined aerobic and resistance exercise training on obese adults, Northwest Ethiopia. Res J Recent Sci. 2013; 2(1): 59–66.
4.
Rudalee Husale, Abhijit Diwate. Effect of obesity on PEFR value. VIMS J Physical Th. 2019; 1(2): 111–116.
5.
Hall JE, Guyton AC. Textbook of Medical Physiology. 12th ed. New York: Elsevier Saunders; 2011. p. 850.
6.
Longo DL, Fauci AS, Kasper DL, et al. Harrison’s principles of Internal Medicine. 18th ed. New York: Mc Graw Hill; 2011. p. 622–633.
7.
Runge MS, Greganti MA. Netter’s Internal Medicine. 2nd ed. Elsevier Saunders; 2008. p 18–28
8.
Saxena Y, Purwar B, Upmanyu R. Adiposity: determinant of peak expiratory flow rate in young Indian adults male. Indian J Chest Dis Allied Sci. 2011; Jan-Mar; 53(1): 29–33. PMID: 21446222.
9.
Saraswathi Ilango, Christy A, Saravanan A, Dr. Prema Sembulingam. Correlation of Obesity Indices with Peak Expiratory Flow Rate in Males and Females. IOSR Journal Of Pharmacy. 2014; 4(2): 21–27.
10.
Patil SR, Mehta A. Comparison of peak expiratory flow rate in obese and non-obese women. Int J Health Sci Res. 2019; 9(9): 39–45.
11.
Sarwari KN, Imtiaz Ali, Jaleeli KA, Shanmukhappa NJ. Assessment of pulmonary functions in young obese males and females in the age group 18–25 years. International Journal of Basic and Applied Medical Sciences. 2012; 2(3): 185–189.
12.
Basuli Goswami, Anindita Singha Roy, Rishna Dalui and Amit Bandyopadhyay, Peak Expiratory Flow Rate – A Consistent Marker of Respiratory Illness Associated with Childhood Obesity. American Journal of Sports Science and Medicine. 2014; 2(1): 21–26. doi: 10.12691/ajssm-2-1- 4.
13.
Price JPK, Arthur N, Macstephen AO. Correlation between Body Mass Index and Peak Expiratory Flow Rate of an Indigenous Nigerian Population in the Niger Delta Region. Res J Recent Sci. 2013; 2(2): 28–32.
14.
Pradeep Prajapatil, Neelima Singh1, Raj Kishori Prajapati2, Jagat Pal Singh. A prospective study of pulmonary function test in obese patient. Int J Adv Med. 2016; 3(1): 73–76.
15.
Rudalee Husale, Abhijit Diwate. Effect of obesity on PEFR value.VIMS J Physical Th. 2019; 1(2): 111–116.
16.
Das, Naba & Sarkar, Gautam & Khan, Ansar. Correlation Between Body Mass Index and Peak Expiratory Flow Rate of an Indigenous Brick Industry Labour on Bank of Kangsabati River, Paschim Medinipur, West Bengal. Indian Journal of Research. 2014; 3: 129–131.
17.
Jena SK, Mirdha M, Meher P, Misra AK. Relation of peak expiratory flow rate to body mass index in young adults. Muller J Med Sci Res 2017; 8: 19–23.
18.
Koraddi ST, Shrilaxmi Bagali, Manjunatha Aithala. Effect of Body Fat Distribution on Pulmonary Functions in Young Healthy Obese Students. JKIMSU. 2015; 4(4): 18–26.
19.
Ajay KT, Vatsala AR, Suresh Y Bondade, Sonam D, Sangam. Effect of obesity on cardiovascular functions in adolescent male. J Pharm. Sci&Res. 2014; 6(3): 164 –166.
20.
Laxmi CC, Udaya IB, Vinutha Shankar S. Effect of body mass index on cardiorespiratory fitness in young healthy males.International Journal of Scientific and Research Publications. 2014; 4(2): 1–3.
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.