REVIEW PAPER
Cardiac Arrest – An interdisciplinary scoping review of preclinical literature from 2020
1
Cardiothoracic Critical Care, Miami Transplant Institute, University of Miami, USA
2
Department of Emergency Medicine, University of Florida, Gainesville, FL, USA
3
Department of Surgery, Yale University, New Haven, CT, USA
4
Lake Erie College of Osteopathic Medicine, Bradenton, FL, USA
Corresponding author
J Pre Clin Clin Res. 2022;16(2):45-53
KEYWORDS
epidemiologyemergency medical servicescardiopulmonary resuscitationheart arrestout-of-hospital cardiac arrestsudden cardiac death
TOPICS
ABSTRACT
Introduction and objective:
The Interdisciplinary Cardiac Arrest Research Review (ICARE) group was formed in 2018 to conduct an annual search of peer-reviewed literature relevant to cardiac arrest. Now in its third year, the goals of the review are to illustrate best practices in research and help reduce compartmentalization of knowledge by disseminating relevant advances in the interdisciplinary world of cardiac arrest research. This iteration focuses on pharmacology and basic and translational science contributions.
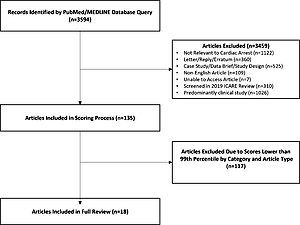
Review methods:
A search was conducted of PubMed using keywords related to cardiac arrest. Titles and abstracts were screened for relevance with a focus on basic science and pharmacology. Screened manuscripts underwent standardized scoring of methodological quality and impact on the respective fields by reviewer teams lead by a subject matter expert editor. Articles scoring higher than 99 percentiles by category were selected for full critique. Systematic differences between editors’ and reviewers’ scores were assessed using Wilcoxon signed-rank test.
Brief description of the state of knowledge:
The top scoring studies centered around attempts at improving neurologic outcome through improved blood flow and reduction of metabolic demand in order to reduce the impact of hypoxia during resuscitation on the brain.
Summary:
The sheer number of articles screened is a testament to the need for an accessible source highlighting highquality and important research. Several high-quality systematic reviews and original research studies have provided a physiologic basis for the treatment of cardiac arrest, and make the case for focused progression of several pharmacologic treatments to larger animal and human trials.
The Interdisciplinary Cardiac Arrest Research Review (ICARE) group was formed in 2018 to conduct an annual search of peer-reviewed literature relevant to cardiac arrest. Now in its third year, the goals of the review are to illustrate best practices in research and help reduce compartmentalization of knowledge by disseminating relevant advances in the interdisciplinary world of cardiac arrest research. This iteration focuses on pharmacology and basic and translational science contributions.
Review methods:
A search was conducted of PubMed using keywords related to cardiac arrest. Titles and abstracts were screened for relevance with a focus on basic science and pharmacology. Screened manuscripts underwent standardized scoring of methodological quality and impact on the respective fields by reviewer teams lead by a subject matter expert editor. Articles scoring higher than 99 percentiles by category were selected for full critique. Systematic differences between editors’ and reviewers’ scores were assessed using Wilcoxon signed-rank test.
Brief description of the state of knowledge:
The top scoring studies centered around attempts at improving neurologic outcome through improved blood flow and reduction of metabolic demand in order to reduce the impact of hypoxia during resuscitation on the brain.
Summary:
The sheer number of articles screened is a testament to the need for an accessible source highlighting highquality and important research. Several high-quality systematic reviews and original research studies have provided a physiologic basis for the treatment of cardiac arrest, and make the case for focused progression of several pharmacologic treatments to larger animal and human trials.
Travis W Murphy, Charles W Hwang, Scott A Cohen, Sarah Gul, Francis Han, Torben K Becker. Cardiac Arrest: An Interdisciplinary Scoping
Review of Preclinical Literature from 2020. J Pre-Clin Clin Res. 2022; 16(2): 45–53. doi: 10.26444/jpccr/150030
REFERENCES (21)
1.
Wong CX, Brown A, Lau DH, Chugh SS, Albert CM, Kalman JM, et al. Epidemiology of Sudden Cardiac Death: Global and Regional Perspectives. Hear Lung Circ. 2019;28:6–14. https://doi.org/10.1016/j.hlc.....
2.
Murphy TW, Cohen SA, Avery KL, Balakrishnan MP, Balu R, Chowdhury MAB, et al. Cardiac arrest: An interdisciplinary scoping review of the literature from 2019. Resusc Plus. 2020;4:100037. https://doi.org/10.1016/j.resp....
3.
Schroeder ED, Jacquet G, Becker TK, Foran M, Goldberg E, Aschkenasy M, et al. Global emergency medicine: A review of the literature from 2011. Acad Emerg Med. 2012. https://doi.org/10.1111/j.1553....
4.
Gul SS, Cohen SA, Avery L, Balakrishnan MP, Balu R, Chowdhury MAB, et al. Cardiac arrest: An interdisciplinary review of the literature from 2018. Resuscitation. 2020;148:66–82. https://doi.org/10.1016/j.resu....
5.
Orso D, Vetrugno L, Federici N, Borselli M, Spadaro S, Cammarota G, et al. Mechanical Ventilation Management During Mechanical Chest Compressions. Respir Care. 2021;66:334–46. https://doi.org/10.4187/respca....
6.
Shoaib M, Choudhary RC, Choi J, Kim N, Hayashida K, Yagi T, et al. Plasma metabolomics supports the use of long-duration cardiac arrest rodent model to study human disease by demonstrating similar metabolic alterations. Sci Rep. 2020;10. https://doi.org/10.1038/s41598....
7.
Zhao Q, Shen Y, Li R, Wu J, Lyu J, Jiang M, et al. Cardiac arrest and resuscitation activates the hypothalamic-pituitary-adrenal axis and results in severe immunosuppression. J Cereb Blood Flow Metab. 2021;41:1091–102. https://doi.org/10.1177/027167....
8.
Liu B, Zhang Q, Li C. Steroid use after cardiac arrest is associated with favourable outcomes: a systematic review and meta-analysis. J Int Med Res. 2020;48. https://doi.org/10.1177/030006....
9.
Olai H, Thornéus G, Watson H, Macleod M, Rhodes J, Friberg H, et al. Meta-analysis of targeted temperature management in animal models of cardiac arrest. Intensive Care Med Exp. 2020;8. https://doi.org/10.1186/s40635....
10.
Lind PC, Johannsen CM, Vammen L, Magnussen A, Andersen LW, Granfeldt A. Translation from animal studies of novel pharmacological therapies to clinical trials in cardiac arrest: A systematic review. Resuscitation. 2021;158:258–69. https://doi.org/10.1016/j.resu....
11.
Piao L, Fang YH, Hamanaka RB, Mutlu GM, Dezfulian C, Archer SL, et al. Suppression of superoxide-hydrogen peroxide production at site IQ of mitochondrial complex I attenuates myocardial stunning and improves postcardiac arrest outcomes. Crit Care Med. 2020;48:E133–40. https://doi.org/10.1097/CCM.00....
12.
Yang M, Hua T, Yang Z, Chen L, Zou Y, Huang X, et al. The Protective Effect of rhBNP on Postresuscitation Myocardial Dysfunction in a Rat Cardiac Arrest Model. Biomed Res Int. 2020;2020. https://doi.org/10.1155/2020/6....
13.
Rysz S, Lundberg J, Nordberg P, Eriksson H, Wieslander B, Lundin M, et al. The effect of levosimendan on survival and cardiac performance in an ischemic cardiac arrest model – A blinded randomized placebo-controlled study in swine. Resuscitation. 2020;150:113–20. https://doi.org/10.1016/j.resu....
14.
Jung YH, Mamadjonov N, Lee HY, Jeung KW, Lee BK, Youn CS, et al. Effects of different doses of pralidoxime administered during cardiopulmonary resuscitation and the role of a-adrenergic receptors in its pressor action. J Am Heart Assoc. 2020;9. https://doi.org/10.1161/JAHA.1....
15.
Yauger YJ, Beaumont DM, Brady K, Schauer SG, O’Sullivan J, Hensler JG, et al. Endotracheal Administered Epinephrine Is Effective in Return of Spontaneous Circulation Within a Pediatric Swine Hypovolemic Cardiac Arrest Model. Pediatr Emerg Care. 2020;Publish Ah. https://doi.org/10.1097/pec.00....
16.
Zhao H, Fan K, Feng G. Amiodarone and/or lidocaine for cardiac arrest: A Bayesian network meta-analysis. Am J Emerg Med. 2020;38:2185–93. https://doi.org/10.1016/j.ajem....
17.
Kudenchuk PJ, Brown SP, Daya M, Rea T, Nichol G, Morrison LJ, et al. Amiodarone, Lidocaine, or Placebo in Out-of-Hospital Cardiac Arrest. N Engl J Med 2016;374:1711–22. https://doi.org/10.1056/nejmoa....
18.
Shen R, Pan D, Wang Z, Jin X, Li Z, Wang H. The Effects of Dexmedetomidine Post-Conditioning on Cardiac and Neurological Outcomes After Cardiac Arrest and Resuscitation in Swine. Shock 2021;55:388–95. https://doi.org/10.1097/SHK.00....
19.
Dogan EM, Hörer TM, Edström M, Martell EA, Sandblom I, Marttala J, et al. Resuscitative endovascular balloon occlusion of the aorta in zone I versus zone III in a porcine model of non-traumatic cardiac arrest and cardiopulmonary resuscitation: A randomized study. Resuscitation. 2020;151:150–6. https://doi.org/10.1016/j.resu....
20.
Nowadly CD, Hoareau GL, Grayson JK, Johnson MA. Zone 3 REBOA does not provide hemodynamic benefits during nontraumatic cardiac arrest. Am J Emerg Med. 2020;38:1915–20. https://doi.org/10.1016/j.ajem....
21.
Duhem H, Moore JC, Rojas-Salvador C, Salverda B, Lick M, Pepe P, et al. Improving post-cardiac arrest cerebral perfusion pressure by elevating the head and thorax. Resuscitation. 2021;159:45–53. https://doi.org/10.1016/j.resu....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.